Immunotherapy has made headlines in the fight against cancer in recent years. We wanted to know from Prof. Dr. med. Markus G. Manz, Head of the Center for Hematology and Oncology at the USZ, how immunotherapy actually works.
Prof. Manz, how does a tumor develop?
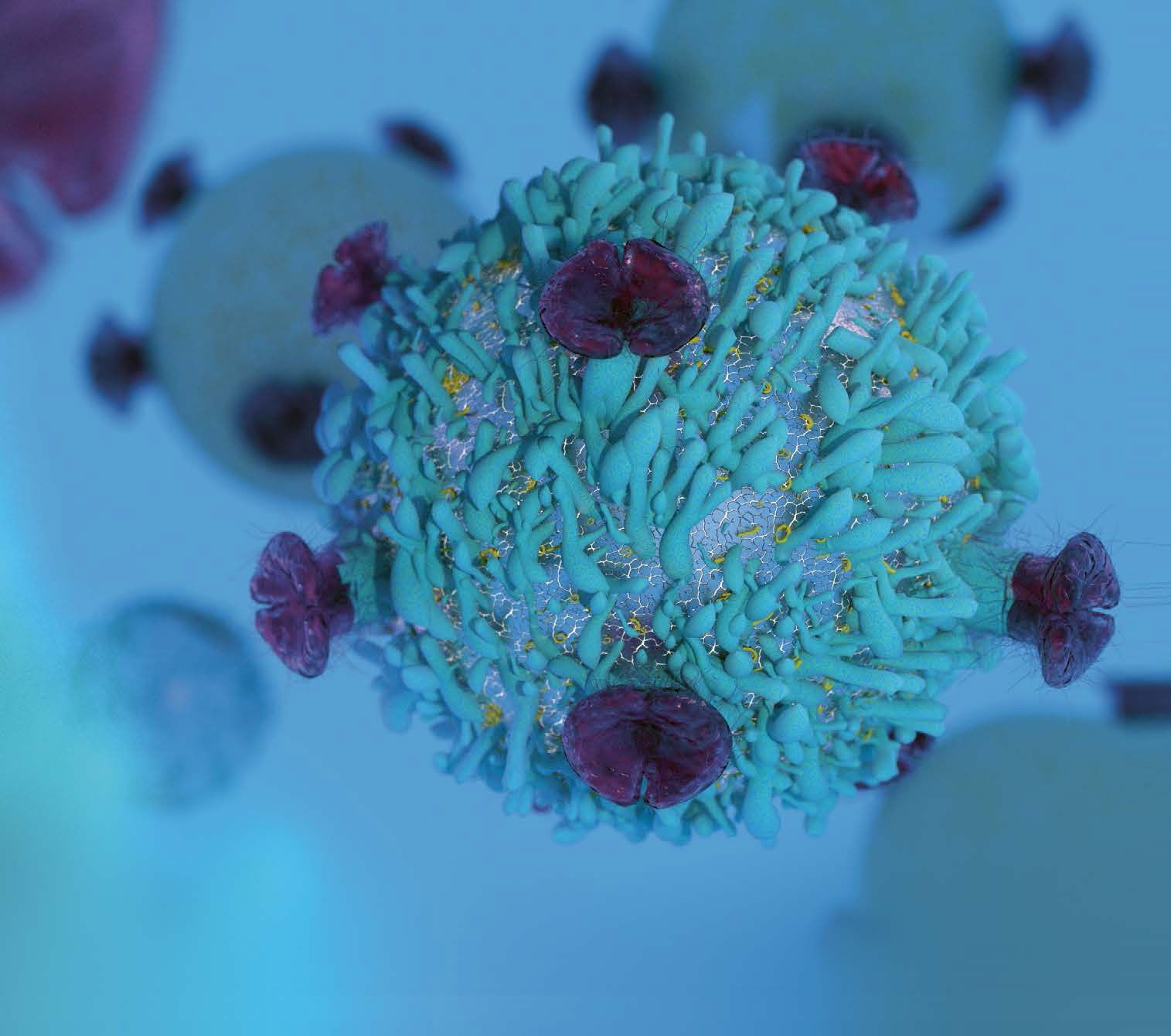
The human immune system protects the body from damage caused by infectious diseases by recognizing “invaders” as foreign and repelling them, but at the same time preserving healthy tissue or allowing it to regenerate. Cancer is first and foremost the body’s own tissue, i.e. not foreign tissue. However, this carries genetic changes that trigger the uncontrolled growth and do not occur in this way in healthy tissue. However, these changes are often subtle, do not show up sufficiently on the tumor cell surface and increase only slowly in type and quantity. This then leads to the fact that the tumors are very similar to healthy tissue and that the patient’s own immune system either cannot recognize the changes at all and is not activated. Or the change is recognized, but the immune response is suppressed, i.e. a kind of immune tolerance occurs. The result is an absent or insufficient immune response and thus a growing tumor.
Today there is often talk of immunotherapy. What does this mean?
Tumor immunotherapy” is an umbrella term for very different approaches that use methods of the immune system to fight cancer. These can either be immunotherapeutic agents administered externally, e.g. as an infusion (e.g. antibodies against tumor cells that are not normally produced by the body in this way) or, in the case of a shutdown of the patient’s own immune system, the immune system can be activated by releasing the “brakes” of the immune system, so to speak, and thus lifting the immune tolerance.
There are different types of cancer therapy. Can you briefly describe these and categorize the immunotherapy?
Other principles of cancer therapy are, roughly summarized, surgery, radiation and classical chemotherapy, as well as the new molecular, targeted therapies, which are aimed at interrupting the cancer-driving changes inside tumour cells.
Surgery is essentially about removing the original tumor. This is the gold standard for many tumors. One problem with this is that it can be associated with severe side effects if the tumor is extensive. If the disease has spread to a large number of sites, i.e. has metastasized, then surgery is, with a few exceptions, no longer an appropriate measure because it causes more harm than good for the patient and a cure is not possible.
The situation is similar with radiotherapy, although great progress has been made in this area too, particularly in cases of limited tumor spread or spread to critical areas, and radiotherapy has become more targeted and has fewer side effects. In the case of extensive metastasis, however, radiotherapy is usually not advisable due to the multiple side effects.
Classic chemotherapy is used either to remove the smallest “tumor remnants” after an operation, for example, or in the case of widespread tumor disease. Chemotherapy is still often the gold standard for widespread tumor disease. Since tumor cells divide much faster than healthy body cells and chemotherapy targets the cell division apparatus, they are easily attacked by chemotherapy. This can often reduce the disease and prolong life. Cures are very rare with widespread disease, even under chemotherapy, or are limited to a few tumor types. The problem with chemotherapy is that it also affects other rapidly dividing tissues. This leads to side effects such as weakening of the hematopoietic system, inflammation of the mucous membranes and hair loss. In addition, metabolic and detoxification organs (such as the kidneys) can also be damaged, i.e. major collateral organ damage can occur.
The molecular, targeted therapies against intracellular tumor drivers and the immunotherapies against molecules on the cell surface have a more specific effect overall. In other words, these therapies represent important steps in the direction of harming only the tumor and sparing the healthy, vital tissue.
How can the body’s own immune system recognize cancer and how is it strengthened?
In the type of immunotherapy that aims to release the brakes on the patient’s own immune system, we aim to strengthen the existing but inactive immune response so that it fights the cancer. The immune response is based on the fact that cancer cells may have a tumor antigen on their surface, i.e., they carry a surface feature that is different from healthy tissue. This allows the tumor cell to be perceived by the immune system as a type of foreign cell. Some tumors have many of these different surface features, while others have few of them. In addition, tumors can also produce specific “brake molecules” for the immune system. It is interesting and logical that immune activation therapy of the patient’s own immune system usually works well precisely in those patients whose tumors carry many different surface features and many of these braking molecules compared to healthy tissue. The tumor immune response then occurs when the brake or control signal – the substances are also known as “checkpoint inhibitors” – is neutralized.
A side effect of this activating immunotherapy can be that the brakes of other immune cells are also released and thus side effects occur that correspond to autoimmune diseases, i.e. that the immune system attacks healthy tissue as well. So there is a problem of selectivity here. However, depending on the type of cancer, the resulting side effects can be accepted and in some cases well controlled. Overall, one can assume fewer and different side effects than with classical chemotherapy.
Targeted immunotherapy at the CCCZ
At the CCCZ, we use targeted immunotherapies to enable the body’s own immune defenses to recognize tumor cells and eliminate them in a targeted manner.
What other types of immunotherapy are currently available?
In addition to the above-mentioned activation of the patient’s own immune system, there are immunotherapies in which structures of the immune system are produced externally. These are then infused. The simplest and classic example is so-called antibodies, which go to tumor cell surfaces and attack them. Either the targets of the antibodies are tumor-specific (this is rare) or the targets are also present on healthy tissues but in lower density, or the tissue can be temporarily dispensed with and it regenerates after therapy.
Recent developments in so-called “designer immunology” show that it is also possible to produce antibodies or antibody fragments to which one can then couple either chemotherapy or radiotherapy or cell messengers and deliver them relatively selectively to the tumor. Similarly, antibodies can be produced that act as an activating bridge between the tumor cell and the body’s own immune cell. That is, these antibodies stimulate the immune cell to kill the tumor cell. Another development is the genetic manipulation of the body’s own immune cells. In this way, antibodies can be introduced into “killer cells” so that they then attack the tumor cells with high selectivity. These include, for example, the so-called CAR-T cells. Another interesting development is the possibility of immunologically activating phagocytes. In combination with immunotherapy, the aim is to clear tumor cells as selectively as possible. There are now exemplary therapies for all these types of immunotherapy that have either already been approved in the clinic or are in early clinical trials.
These therapies are also not without side effects. For example, the massive artificial activation of the immune system can trigger conditions similar to blood poisoning, i.e. high fever and circulatory weakness. This can be dangerous, but there are already countermeasures that are effective.
How does the USZ use immunotherapy?
All the immunotherapy methods mentioned above, including CAR T-cell therapy and phagocyte-activating therapy, are used at the USZ. This therapy, which activates the patient’s own immune system, is used very successfully today, particularly in the fight against black skin cancer (melanoma) and lung cancer. In the field of CAR T-cell therapy and bispecific, T-cell activating antibody therapy, the focus is particularly on lymphomas and plasma cell diseases. We conduct preclinical research on antibody engineering and CAR T cells, e.g. also in a clinical research focus together with the University of Zurich and ETH.