Overview: What is ulcerative colitis?
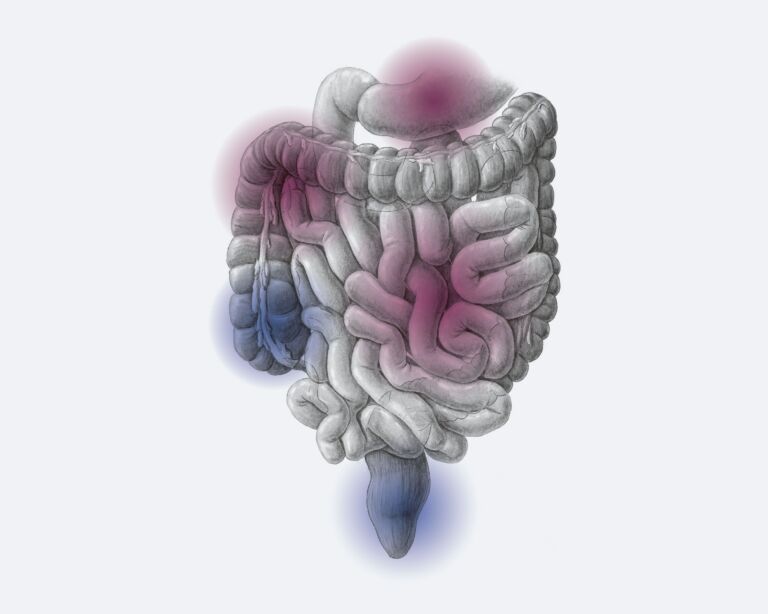
Ulcerative colitis is a chronic inflammatory bowel disease. Typically, it often progresses in relapses, with periods of disease alternating with symptom-free periods with episodes of inflammation. Ulcerative colitis affects only the colon and remains confined to the uppermost layer of the intestinal wall, namely the intestinal mucosa. There, „ulcers“ form, i.e. wounds and shallow defects in the mucosa. The Latin term „ulcus“ means „ulcer“, while „colitis“ stands for inflammation of the large intestine (colon). This is where ulcerative colitis gets its name. Ulcerative colitis always begins in the last section of the large intestine, the rectum, and is worst there. From there, it can spread to other areas of the colon to varying degrees. In severe cases, it may even involve the entire colon. Like Crohn’s disease, ulcerative colitis belongs to the group of chronic inflammatory bowel diseases (IBD). They are the most important main representatives that doctors summarize under the collective term IBD or IBD.
Ulcerative colitis – frequency and age
Chronic inflammatory bowel disease (IBD) is one of the most common diseases in Switzerland: Around one in 350 people suffer from it. This corresponds to more than 25,000 people. Men and women develop ulcerative colitis at about the same rate. Most often, the disease first appears in young adults between the ages of 25 and 35. However, younger people such as young children or senior citizens can also fall ill. A „senile colitis“ is also known, which occurs in elderly people.
Differences in Crohn’s disease
Like Crohn’s disease, ulcerative colitis is a chronic inflammatory bowel disease. Even though the symptoms such as diarrhea and abdominal pain are very similar in both diseases, there are some differences. Crohn’s disease is characterized by the following features:
- The disease can affect the entire gastrointestinal tract – from mouth to anus.
- The sites of inflammation are not related, but may occur in sections in different parts of the intestine. In between, there are always healthy sections of intestine.
- The inflammation usually affects all layers of the intestinal wall, not only the superficial intestinal mucosa. Thus, the inflammation penetrates much deeper into the intestinal layers.
- In half of those affected, short-circuit connections from intestine to intestine or from intestine to skin, so-called „fistulas“, form in the course of the disease.
Therapy by specialists
Ulcerative colitis is a chronic inflammation of the colon that occurs in episodes and requires a graded treatment approach. In the majority of cases, the disease can be successfully controlled with drug therapy, which the gastroenterologist finds together with the patient and adjusts during the course of the disease. Only in rare and severe cases with no or insufficient response to drug therapy, surgical therapy may be the best solution. At the USZ, there is a team of proven specialists with many years of experience in the medicinal and surgical treatment of ulcerative colitis.
Ulcerative colitis: causes and risk factors
The causes of ulcerative colitis have not yet been determined. However, researchers believe that several factors must be at work for inflammatory bowel disease to develop. Possible triggers that play a role in its development are:
- Altered intestinal mucosa: In people with ulcerative colitis, the protective mucus layer on the intestinal mucosa is often thinner than in healthy people. Its defense function is impaired and it has less resistance to pathogenic germs. This makes it easier for bacteria to overcome the (normally protective) intestinal barrier and penetrate the intestinal mucosa. The immune system sends defensive patrols and inflammation occurs.
- Genes: ulcerative colitis is clustered in some families. This suggests that hereditary factors are involved. The risk of disease is higher for close relatives. However, the genetic predisposition plays a smaller role in colitis than in Crohn’s disease and is relevant for at most one in ten cases.
- Environmental factors: Researchers discuss environmental factors and improved hygiene standards as possible contributors because disease rates are climbing in Western industrialized countries and also rising sharply in countries that are adopting Western lifestyles, such as urban areas in China.
Symptoms of ulcerative colitis
Ulcerative colitis can cause unpleasant symptoms during an acute flare. The more extensive the inflammation, the more pronounced the symptoms can be. Possible symptoms of ulcerative colitis:
- Diarrhea, which is often bloody and/or mucousy
- Abdominal pain or cramps, often in the left lower abdomen
- Frequent urge to defecate and the feeling of having to defecate, sometimes very urgently to uncontrollably
- Nocturnal bowel movements, frequent bowel movements of up to 20 times per day
- Pain before or after bowel movement
- Feeling of being bloated
- Loss of appetite
- Weight loss
- Tiredness and fatigue
- Decreased performance, physical weakness
- Fever
- anemia and iron deficiency due to blood loss with bowel movements
Diagnosis ulcerative colitis
We will first ask you some questions about your medical history (anamnesis) to get a first impression. Some examples:
- What exactly are the symptoms you suffer from? Abdominal cramps, blood and mucus in the stool?
- How often do you have diarrhea, how often is there blood involved, and do the bowel movements occur at night?
- How long have the complaints existed and how pronounced are they?
- Are there symptom-free periods in between?
- Do you have any known illnesses, for example an intestinal infection, food intolerance or food allergy?
- Are you taking any medications? If yes: Which and since when?
- Do you have a family history of inflammatory bowel disease? Parents, siblings?
These and other questions help us to make an initial assessment. Further tests then follow to differentiate ulcerative colitis from Crohn’s disease or other diseases.
Other diagnostic methods
Often, the diagnosis of ulcerative colitis can be made after these tests. Sometimes other diagnostic methods follow if the result is inconclusive. These include, for example, magnetic resonance imaging (MRI, magnetic resonance imaging) or endoscopy of the esophagus, stomach and duodenum. It has the name esophagogastroduodenoscopy.
Ulcerative colitis: prevention, early detection, prognosis
The causes behind ulcerative colitis are not yet known. Therefore, it is also not possible to effectively prevent the intestinal disease. Breastfeeding appears to reduce the risk of ulcerative colitis to some extent. Those who were breastfed for at least six months as a baby are less likely to develop the bowel disease than a „bottle-fed“ baby. It has not yet been proven whether the diet has a protective effect. In ulcerative colitis, early detection plays a role in that sufferers have an increased risk of colorectal cancer. In general, it can be said that ulcerative colitis that is discovered in time can often also be better treated. This reduces the risk of possible complications.
Course and prognosis in ulcerative colitis
Ulcerative colitis is a disease that usually progresses in phases. Phases in which the disease is active alternate with symptom-free periods. How often these relapses occur and how intense they are varies from person to person and depends, of course, on the correct and individually adapted therapy. Some experience only a few episodes over the course of their lives, while others catch them several times a year. Sometimes the intestine remains permanently severely inflamed. Then surgical removal of the colon is the correct and necessary measure. Fortunately, thanks to improved medications, this is now only the case for less than one in ten sufferers in Switzerland. It is important to get adequate treatment for ulcerative colitis. In addition, take advantage of regular examinations for the early detection of colorectal cancer. Life expectancy is then similar to that of the normal population.
Complications of ulcerative colitis
As the disease progresses and the ulcerative colitis spreads, some complications can develop. Sometimes an acute disease flare-up is also particularly severe and severe. Doctors refer to it as „fulminant colitis.“ These complications are possible with ulcerative colitis:
- Toxic megacolon: This is a severe inflammation of the entire intestinal wall, which causes the intestine to be considerably stretched – the intestine can rupture, which is life-threatening. We need to operate immediately.
- Intestinal perforation: It means danger to life and a quick operation is necessary.
- Intestinal bleeding: They may result from the severe inflammation. In severe cases, surgery is sometimes necessary.
- Colorectal cancer: People with ulcerative colitis have an increased risk of colorectal cancer, which is why you should have regular cancer screening. The most important measure is colonoscopy. This allows us to detect and treat precancerous lesions or colorectal cancer in time. Discuss with your doctor at what intervals colonoscopy is appropriate. Your personal risk of colorectal cancer depends, for example, on how extensive and severe the inflammation is, whether close family members have had colorectal cancer, whether you have already been found to have colorectal cancer precursors, or whether you have other risk factors for colorectal cancer (e.g. chronic inflammation of the bile ducts, primary sclerosing cholangitis).
Self-help groups
Talking to people with the same condition can be a great support when coping with an illness. Advice on finding a suitable self-help group is available from Selbsthilfe Zürich. Self-Help Zurich and the University Hospital Zurich are cooperation partners in the national project „Health literacy thanks to self-help-friendly hospitals“.
Ulcerative colitis: treatment with different strategies
Ulcerative colitis is a chronic disease that cannot be cured, but can usually be treated very well. It is important that experts are consulted for treatment. We usually combine several treatment approaches to increase effectiveness. The therapies are intended to reduce inflammation, alleviate symptoms, prevent new relapses, extend the time between two relapses, and prevent complications and late effects. This often allows for a symptom-free everyday life with a good quality of life. As a rule, you can also pursue your profession.