Overview: What is sarcoidosis?
Sarcoidosis, also known as Boeck’s disease, is a granulomatous disease. Its classic characteristic is microscopically small, nodular tissue changes. It is unclear why they form. It is probably a dysregulation of the immune system caused by hereditary factors in combination with certain environmental influences.
People suffering from sarcoidosis can have general symptoms that occur with all inflammatory diseases:
- Fever
- Fatigue and exhaustion
- Fatigue
- Weight loss
- Night sweats
- Pain in the limbs
The other symptoms of the disease can vary greatly and depend on which organs are involved.
These are for example:
- Lungs (90 percent)
- Lymph nodes (up to 90 percent)
- Skin
- Joints
- Heart
- Kidney
- Liver
- Spleen
- Eyes
- Bones
- Nervous system
- Salivary gland
Although sarcoidosis most commonly affects the lungs and lymph nodes, it can occur in practically any organ. Experts therefore also refer to it as a systemic disease. If the sarcoidosis affects the lungs, for example, the affected person suffers from a cough and/or shortness of breath. In the case of lymph node infestation, patients occasionally notice swelling of the affected lymph nodes. Sarcoidosis appears in both acute and chronic forms and is not contagious.
Sarcoidosis usually develops between the ages of 20 and 40. Overall, around 20 to 40 out of every 100,000 people suffer from it, women slightly more often than men. Sarcoidosis is significantly more common in some countries, including Sweden and Iceland, and in some population groups, such as US-Americans of black African descent. In addition to hereditary factors, environmental factors are also a possible cause of this accumulation.
Causes and risk factors of sarcoidosis
It is still unclear why some people develop sarcoidosis. However, experts suspect that a hereditary disposition in combination with certain environmental factors can cause the condition.
Hereditary factors
The causes of the chronic inflammatory disease may be genetic factors. factors into consideration. Familial clusters have been described in five percent of cases. In addition, certain genetic changes have been identified that increase the risk of sarcoidosis.
Inhaled pollutants
In nine out of ten cases, sarcoidosis affects a person’s lungs. Researchers therefore assume that the disease is caused by harmful substances that are inhaled (so-called inhalative noxae). It is assumed that the inhaled substances activate the immune system and thus trigger the characteristic nodule formation. The lungs can be affected from the outset or as the disease progresses. Various substances are suspected of triggering sarcoidosis:
- Chemicals
- Particulate matter
- Bacteria
- Mushrooms
- Viruses
- allergenic substances (e.g. pollen)
Symptoms: No clear signs of illness
The symptoms caused by the disease depend on the organs affected, the severity and the course of the disease.
Acute sarcoidosis
In only about ten percent of all cases of the disease do the symptoms appear suddenly. The lungs are usually affected. The usual characteristics of the acute form are
- Fever and general feeling of illness,
- painful, initially red, later bluish nodules under the skin (erythema nodosum), usually on the shins,
- painful swelling and inflammation of the joints (arthritis), usually in the ankle joints,
- Lymph node swelling in the area of the main bronchi and the large pulmonary vessels. The swellings usually do not cause any symptoms, but can be identified on an X-ray.
Chronic sarcoidosis
In around 90 percent of cases, sarcoidosis occurs in its chronic form. It usually affects the lungs and neighboring lymph nodes, although some sufferers do not even notice the disease. In others, the symptoms develop gradually, mainly with an increasing dry cough and shortness of breath on exertion. On the X-ray, we can see the swollen lymph nodes in the lung region. Other signs of the chronic form of sarcoidosis are
- Mild fever
- Weight loss
- Night sweats
- Fatigue
- Joint pain (arthritis)
Sarcoidosis symptoms – possible throughout the body
In principle, sarcoidosis can affect your entire body (extrapulmonary sarcoidosis). The symptoms vary depending on which organ is affected:
- Eyes:Inflammation of various areas of the eyes, such as the iris or the ciliary body, to which the lens of the eye is attached. Eye pain then occurs, especially in bright light.
- Skin: Skin changes, such as erythema nodosum, see above. In addition, bluish-purple skin discoloration can occur (lupus pernio), especially on the cheeks and nose.
- Heart: If the organ is severely affected, sarcoidosis can trigger cardiac insufficiency or cardiac arrhythmia. There is then a risk of serious complications.
- Liver and spleen:Sarcoidosis of these organs can restrict their function. The liver values in the blood may also be altered.
- Kidneys:An increased concentration of calcium in the blood and therefore also in the urine can lead to increased kidney stone formation and calcification of the kidneys (nephrocalcinosis). Sarcoidosis can also manifest itself in the kidneys as an inflammatory disease.
- Central nervous system: Neurosarcoidosis affects the brain and spinal cord. It can cause a loss of cranial nerves and thus paralyze the facial muscles. The disease often also leads tomeningitis.
- Early childhood sarcoidosis: It manifests itself with even less specific symptoms, such as fever, loss of appetite, fatigue and even enlargement of the liver and spleen.
Sarcoidosis: Diagnosis with us
As sarcoidosis manifests itself with different symptoms, its diagnosis is not trivial. If there is any suspicion, the first step is to ask about the possible symptoms. During the physical examination, the lungs, lymph glands and skin are the most frequently affected areas. We will listen to and palpate your chest, inspect your skin closely and may even take a tissue sample to check for nodules. We can also use the following methods for diagnosis:
Lung examination for sarcoidosis
The extent to which sarcoidosis affects the lungs can reach different stages.
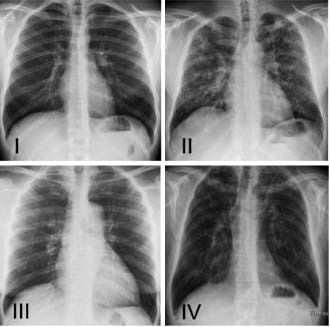
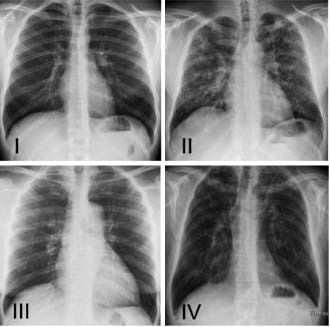
The X-ray findings of the chest show how far the sarcoidosis has progressed:
- Stage 0: symptoms outside the chest, no lung involvement
- Stage I: Swollen lymph nodes between the two lungs. The lung tissue shows no abnormalities. Spontaneous healing rate approx. 70 percent
- Stage II: Swelling of the lymph nodes in the chest plus patchy changes in the lungs. Spontaneous healing rate of around 50 percent
- Stage III: Changes in the lung tissue, but no swelling of the lymph nodes
- Stage IV: Pathological connective tissue remodeling of the lung tissue (pulmonary fibrosis) with impaired lung function
If the lungs are affected, we check the extent of the impairment with the so-called lung function test. A lung endoscopy (bronchoscopy) or an endoscopy of the region between the two lungs (mediastinoscopy) then provides even more differentiated results. During lung endoscopy, we take tissue samples to test for pathological changes.
Blood test for sarcoidosis
There are no specific blood values that confirm or rule out the diagnosis of sarcoidosis. Nevertheless, various laboratory values are used to assess inflammatory activity (e.g. ACE (angiotensin converting enzyme), active vitamin D3, calcium concentration in the blood, neopterin, s-IL2 receptor, CRP, TNF-alpha, the sedimentation rate of blood cells or calcium excretion in the urine).
Imaging techniques
The cross-sectional images of a high-resolution computer tomography (CT ) of the chest allow tissue changes in the lungs and lymph nodes to be detected even more precisely. Positron emission tomography (PET) is often used to determine the spread of sarcoidosis and its activity. The central nervous system can also be examined by CT in the case of sarcoidosis. The method is then supplemented by magnetic resonance imaging.
Sarcoidosis: Examination of other organs
To find out whether sarcoidosis has affected other organs, we can carry out further examinations. For example, we will
- Determine your liver values,
- test the urine and kidney function in the blood and, if necessary, perform a kidney ultrasound and possibly a kidney biopsy
- Examine your heart with electrocardiogram, ultrasound, magnetic resonance imaging (cMRI) or cardiac PET,
- recommend an ophthalmologic examination.
Self-help groups and advice centers
The exchange with people who are affected by the same disease can be a great support in coping with the disease. Advice on finding a suitable self-help group is available from Selbsthilfe Zürich. Self-Help Zurich and the University Hospital Zurich are cooperation partners in the national project “Health literacy thanks to self-help-friendly hospitals”.
Sarcoidosis: prevention, early detection, prognosis
As the causes of sarcoidosis are not yet fully understood, it is not possible to prevent the disease. Early detection of sarcoidosis is also difficult due to the non-specific symptoms.
Despite its sometimes severe symptoms, the prognosis for acute sarcoidosis is very good: a high proportion of those affected experience a spontaneous recovery within the first four to six weeks. After one year, the changes in the lungs detected during the X-ray examination have regressed.
The prognosis for the chronic form of sarcoidosis is somewhat less favorable. However, in around 70 out of 100 people with chronic stage I sarcoidosis, the disease heals spontaneously within two years. However, the spontaneous healing rate decreases with increasing severity of the disease (see above). However, some chronic cases of sarcoidosis heal after a single course of immunosuppressive therapy. However, if the heart, brain or lungs are severely affected, there is an increased risk of dying from sarcoidosis.
Complications due to sarcoidosis
Various complications can occur as a result of chronic sarcoidosis.
- Paralysis,
- Lung scarring (pulmonary fibrosis),
- Heart failure or cardiac arrhythmia
- Rarely renal dysfunction,
- Visual disturbances.
Sarcoidosis: treatment not always necessary
It is not always necessary to treat sarcoidosis. If you have mild sarcoidosis with a favorable prognosis, you can initially wait with treatment, although you should visit us regularly for check-ups.
Drug treatment for sarcoidosis
There are several active substances that we can use to treat sarcoidosis:
- Cortisone: If drug therapy is necessary, glucocorticoids, of which prednisone is the best known, are particularly suitable. They help very well, but serious side effects can occur during long-term therapy. Therefore, one of the following criteria should be met before we use cortisone in tablet form: You suffer from severe symptoms.
- This is stage II sarcoidosis, from which the lung function deteriorates.
The initial sarcoidosis therapy with cortisone lasts around four to twelve weeks. We then gradually reduce the dosage. We will discuss discontinuing the therapy after six months at the earliest.
- Local cortisone preparations: For the treatment of eyes or skin, cortisone preparations can also be used locally in the form of eye drops or ointment in the case of sarcoidosis. For the treatment of the lungs, it may be possible to switch to an inhalation spray after initially taking tablets.
- Immunosuppressants: If the sarcoidosis takes a protracted course or the cortisone therapy is not effective enough, we can also give you medication against the body’s own defense system (immunosuppressants), for example azathioprine, methotrexate or a TNF-alpha blocker (infliximab or adalimumab).
- Lung transplantation: If the connective tissue of the lungs has been scarred at an advanced stage and the function of the lungs is restricted(pulmonary fibrosis), the last treatment option is a lung transplant.