What are osteoporotic fractures?
Osteoporotic fractures are bone fractures caused by bone loss – osteoporosis. In this disease, those affected increasingly lose bone mass and their bone density decreases. In addition, the microarchitecture of the bone changes – it remodels and loses its strength. The actually solid “supports” of the body become unstable, porous and break more easily over time.
In principle, osteoporotic fractures can affect every single bone in the body. However, the vertebral bodies, femoral neck, upper arm and forearm near the wrist often break. The bones often splinter at the slightest strain, such as a coughing fit or carrying a shopping bag. Sometimes they also break spontaneously without any reason.
An osteoporotic fracture usually manifests itself through pain. However, the fracture can also be completely painless and patients do not even notice it. Swelling, bruising and limited mobility are also indications of a broken bone.
Treatment depends on exactly which bone is broken and the severity of the fracture. A person’s age and general state of health also play a role in the choice of therapy. In many cases, conservative treatment without surgery helps, for example with the help of casts, splints, corsets and physiotherapy. Doctors can also reattach the bone during an operation. Surgery is usually unavoidable in the case of a femoral neck fracture.
Osteoporotic fractures – frequency and age
Around 400,000 people in Switzerland suffer from osteoporosis. As in other countries, women are much more frequently affected by bone loss than men. This is partly due to female hormones. The lack of oestrogen during the menopause has an unfavorable effect on bone metabolism and bone stability.
Osteoporosis is a disease that mostly affects older people. Sometimes the disease also occurs at a younger age. The probability of suffering a bone fracture due to osteoporosis after the age of 50 is 51 percent on average for women and 20 percent for men in Switzerland.
Osteoporotic fractures: causes and risk factors
The cause of osteoporotic fractures is bone loss – osteoporosis. In this disease, bone density decreases and bone mass decreases. In addition, the architecture of the bone changes – it loses its strength and becomes porous, unstable and breaks more easily.
Bone is a very lively tissue that is constantly busy. Special cells – the osteoblasts – build up the bone substance. Their counterparts – the osteoclasts – on the other hand, cause the bone to break down. At a young age, bone formation predominates. Bone-building and bone-degrading processes then roughly balance each other out. From around the age of 40, however, the degradation processes predominate and bone density decreases. However, osteoporosis is only present when the balance has clearly shifted in favor of bone resorption. And then the risk of an osteoporotic fracture increases.
The fracture can occur as a result of mechanical force, for example if a person trips and falls over the carpet or when going to the toilet at night. Sudden attacks of dizziness can also cause a fall. And those who carry heavy loads also have an increased risk of an osteoporotic fracture.
However, sometimes it doesn’t take much force to break a bone that has been weakened by osteoporosis. The fracture often occurs slowly, for example when one or more vertebral bodies gradually collapse. The bone then breaks spontaneously due to the body’s own stress. And the more a bone is weakened by osteoporosis, the higher the risk of fracture.
Osteoporotic fractures – these bones are often affected
The risk of osteoporosis-related fractures is particularly high in these bones:
- Vertebral bodies: The majority of osteoporotic fractures occur in the vertebral bodies, which form the basic framework of the spine. The thoracic and lumbar vertebrae are usually affected. There are three different types of vertebral fractures – depending on the severity and shape of the fracture. In the “fish vertebra“, the central part of the vertebra is sunken in. Because the vertebra gives way in the middle, it is flatter there than at the edges. The rear section, on the other hand, remains largely undamaged. Doctors speak of a “wedge vertebra” when the forward-facing part of the vertebra is collapsed. The front edge is therefore flatter than the rear edge. The term “flat or compression vertebra” is used when the entire vertebra has collapsed.
- Thigh, mostly femoral neck fracture
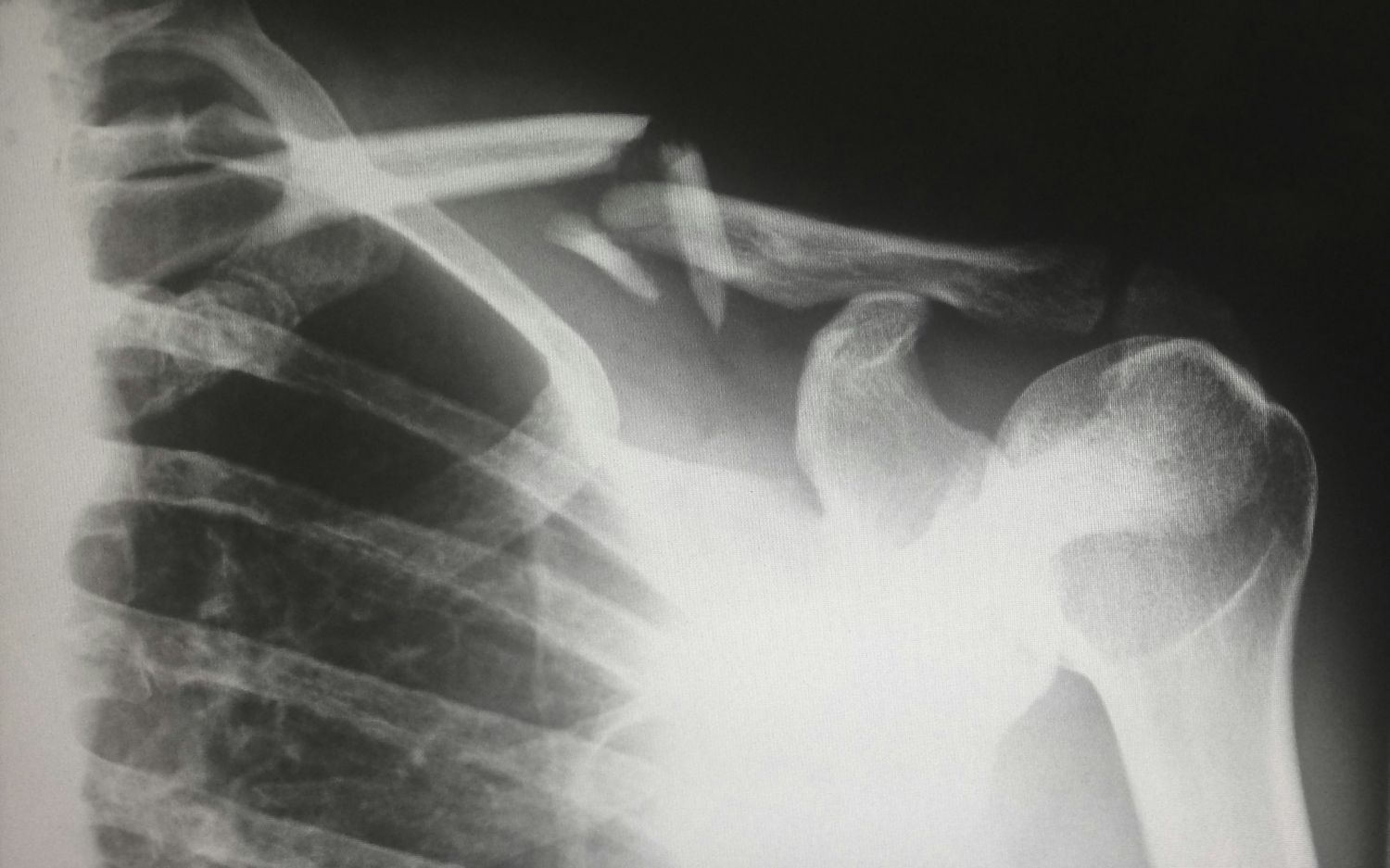
- Upper arm – often humeral head fracture near the shoulder
- Forearm, usually radial fracture close to the wrist
- Pelvic fracture
- Hip fracture
Incidentally, doctors often only discover osteoporosis after a bone fracture. The fracture is then the first indication of bone loss.
Osteoporotic fractures: risk factors
A number of risk factors are known which can presumably increase the risk of osteoporotic fractures to varying degrees. Some examples:
- General risk factors: e.g. older age, female gender, vertebral fractures, fractures after the age of 50 that do not affect the spine, fractures of the femoral neck in the mother or father or multiple falls without external cause
- Underlying diseases: e.g. metabolic diseases (e.g. e.g. diabetes mellitus), hormonal diseases (e.g. Cushing’s syndrome, etc.), rheumatic diseases (e.g. B. rheumatoid arthritis), gastrointestinal diseases (e. g. B. celiac disease, chronic inflammatory bowel diseases such as Crohn’s disease), neurological diseases (e. g. B. Epilepsy)
- Medication: e.g. hormone therapy (for men with prostate cancer), aromatase inhibitors (for women with breast cancer), glucocorticoids (“cortisone”) or medication that promotes falls
Symptoms: Osteoporotic fractures are usually painful
In most cases, the symptoms of an osteoporotic fracture are more or less severe pain. How intense they are and on which part of the body they appear depends on the bone that is broken. The fracture of a larger bone in the thigh, upper arm or forearm usually causes more severe pain. In contrast, the fracture of a single vertebral body can cause less pain and go unnoticed for a longer period of time. However, if several vertebral bodies have collapsed, most people experience chronic back pain.
The pain can be accompanied by other symptoms, for example
- Swelling in the area of the fracture
- Bruises (hematomas)
- Limited mobility
- Reduced or absent resilience
- In the case of vertebral fractures: Round back (“humpback”), decrease in height, altered posture, lung problems and difficulty breathing (if thoracic vertebrae are affected)
- Sometimes audible and painful bone rubbing
- Abnormal position of the affected limb
If you experience such symptoms, always visit your doctor’s surgery immediately or contact the emergency services. Particularly in older people, severe pain after a fall or impact with a hard object is always an alarm signal. It could be an osteoporotic fracture.
Osteoporotic fractures: Diagnosis with us
The diagnosis of an osteoporotic fracture begins with a discussion of your medical history, the anamnesis. We will ask you a few questions to find out the cause of your symptoms, for example:
- What exactly are your symptoms?
- How long have you had the complaints?
- How intense are the symptoms, for example the pain?
- Where exactly would you localize the complaints?
- Did the symptoms develop gradually or did they start suddenly?
- Can you name a triggering event, such as a fall?
- Do you have any known underlying conditions, such as osteoporosis or other illnesses?
- Are you taking any medications? If yes: Which and since when?
- Have you ever had a vertebral body fracture or other bone fracture?
Based on your answers, we can already draw initial conclusions about the disease. This is followed by a physical examination, during which we palpate the body with our hands and detect changes (e.g. swelling). We also pay attention to your posture and height and check your mobility. A neurological examination to test the function of the nerves and muscles is also helpful in the case of vertebral body fractures. Sometimes nerves are crushed during a vertebral fracture.
Osteoporotic fractures can be diagnosed with the help of imaging techniques. To be used:
- X-ray examination: Bone fractures of any kind are usually easily recognizable on an X-ray. We can see the exact location and extent of the fracture.
- Computed tomography (CT): This method also works with X-rays and images the body “slice by slice”. We obtain detailed sectional images of the inside of the body. The CT images also show whether nerves have been crushed in vertebral body fractures, for example.
- Magnetic resonance imaging (MRI = magnetic resonance imaging): This procedure works with strong magnetic fields and also provides high-resolution sectional images. It also shows the condition of the ligaments, intervertebral discs and nerves in the case of vertebral body fractures.
If osteoporosis has not yet been diagnosed, we carry out a bone density measurement (osteodensitometry). There are also other methods for diagnosing bone loss.
Osteoporotic fractures: prevention, early detection, prognosis
There are a number of measures that you can take to prevent osteoporotic fractures. They are particularly important for older people. It is best to discuss with your doctor which measures make sense for you.
Some tips:
- Exercise regularly and be physically active. For example, go for brisk walks more often. This strengthens your muscles and keeps your joints flexible. Endurance sports such as swimming, cycling, hiking or Nordic walking are also good.
- Strength training strengthens the muscles and can help prevent osteoporotic fractures.
- You can also train your balance and coordination. This also helps you to remain stable and sure-footed.
- Eat as healthy and balanced a diet as possible to keep your bones strong. It is important that you get enough protein, calcium and vitamins from your diet. A sufficient supply of vitamin D, for example, is important.
- Give up smoking and if you are a smoker: Try to stop smoking. And if it doesn’t work at the first attempt, try again.
- Only drink alcohol in moderation or avoid alcoholic drinks altogether if possible.
- Fall prevention: Eliminate tripping hazards in your home. This includes, for example, cables, carpets, runners or door thresholds. If necessary, seek professional advice from a specialist. Some organizations offer help with fall prevention, for example the Rheumaliga Schweiz.
- Some medications can increase the risk of falling. Talk to your doctor about whether you really need all the medicines and what interactions they have.
There are also options for the early detection of osteoporotic fractures. If you suffer from osteoporosis, you should adhere as closely as possible to your therapy and attend regular check-ups at your doctor’s surgery. Doctors can recognize whether bone loss is progressing and to what extent. A bone fracture due to osteoporosis, such as a vertebral fracture, can often be detected at an early stage. Regular monitoring is also important if you have certain risk factors for osteoporotic fractures, such as an underlying disease or are taking certain medications.
Otherwise, the general advice is to always visit your doctor’s surgery promptly if you suffer from symptoms such as pain, swelling or redness. A visit to the doctor is also advisable if you suffer from chronic back pain, for example. This could be due to vertebral fractures.
Progression and prognosis of osteoporotic fractures
The course and prognosis of a bone fracture due to osteoporosis cannot be generally predicted. Both depend on which bone is broken. A femoral neck fracture can be particularly serious in older people. It can lead to subsequent disability, the need for care and a reduced quality of life. In the case of vertebral fractures, for example, it is important for the prognosis how many vertebral bodies have collapsed and at what point. Your age, general physical condition and existing underlying illnesses also influence the prognosis.
If doctors recognize and treat the osteoporotic fracture at an early stage, the chances are good that the fracture will heal. However, after a fracture there is a four to five times higher risk of a further fracture. As a rule, a fracture is not the only cause, because other bones are also weakened and brittle due to bone loss.
Osteoporotic fractures: treatment with or without surgery
The treatment of an osteoporotic fracture depends on which bone is affected and how severe the injury is. The general state of health, existing illnesses and age also play a role in the therapy. The aim of the treatment is for you to become as active and mobile again as you were before the fracture. Doctors generally differentiate between conservative treatment methods (without surgery) and treatment with the help of a surgical procedure.