These early signs usually disappear again at the beginning. Over time, it can lead to increasing limitations and disabilities, and the relapsing-remitting course often turns into a so-called secondary progression after 10 – 15 years, during which neurological deficits can steadily worsen and the relapses become less frequent or disappear. Nevertheless, many sufferers are still able to work even after a long period of illness and can continue their lives without major restrictions. There is currently no cure for the disease. However, a whole range of treatments are available today, some of which are highly effective, which can slow down the progression, prevent acute symptoms and signs of the disease and shorten relapses. Even as an affected person, you can do a lot to maintain your quality of life.
Multiple sclerosis (MS)
MS, encephalomyelitis disseminata, ED
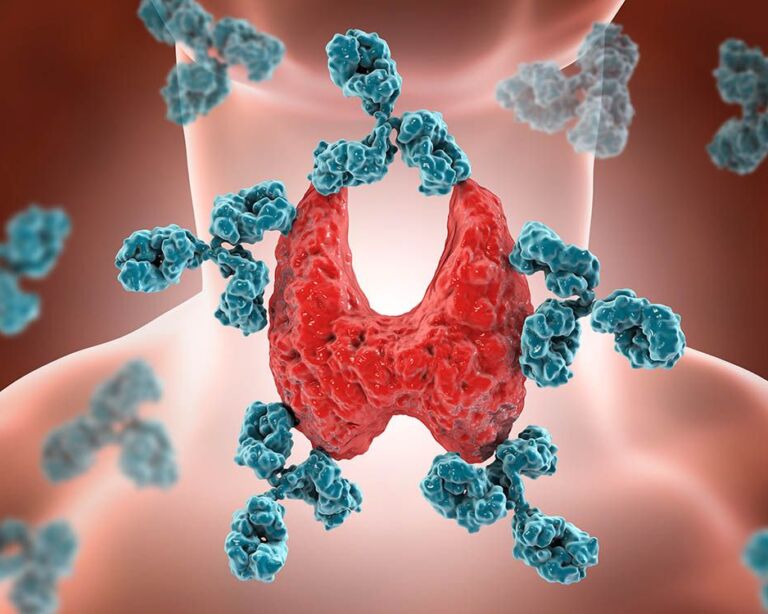
Multiple sclerosis (MS) is an autoimmune, chronic inflammatory disease of the central nervous system. MS usually progresses in relapses and can take different forms. Temporary sensory disturbances, visual disturbances and muscle paralysis are the most common early signs.

Definition of multiple sclerosis
Multiple sclerosis (MS) is a chronic inflammatory disease of the central nervous system (CNS). The central nervous system includes the brain and spinal cord. In multiple sclerosis, inflammatory cells, so-called T and B lymphocytes in the brain and spinal cord destroy the sheathing of the nerve fibers, the so-called myelin, and also the nerve cells and their projections. As the attack is directed against the body’s own tissue, multiple sclerosis is an autoimmune disease.
The term multiple sclerosis is derived from the Latin word “multiple” = “many” and the Greek word “skleros” = “hard”. Doctors also refer to the disease as encephalomyelitis disseminata (ED). This translates as “an inflammation scattered throughout the brain and spinal cord”.
The protective layer of the nerve fibers, the so-called myelin sheaths, ensure that stimuli sent by the brain cells to the various regions of the body are transmitted very quickly. The inflammation damages the myelin at the sites of inflammation, which can temporarily interrupt or slow down nerve conduction. This can manifest itself in the symptoms mentioned. As a result, scar tissue forms in these areas. This pathological hardening of the tissue is called sclerosis.
The affected areas, known as plaques, occur particularly frequently on the optic nerves, in the brain stem, in the cerebellum and on the posterior cords of the spinal cord. The transmission of excitation is disturbed at these points. The nerve fibers themselves are also damaged to a greater or lesser extent. As a result, electrical impulses from the nerve cells only reach the body cells (e.g. muscle cells) and back to a limited extent. As a result, body movements (motor function) and body sensations (sensory function) may be impaired. This is noticeable, among other things, through symptoms of numbness or paralysis.
Multiple sclerosis: causes and risk factors
The causes of multiple sclerosis are not yet known in detail. Both genetic components with a large number of immunologically relevant genes and environmental factors such as smoking, low vitamin D3 levels, infection with the Epstein Barr virus and obesity in adolescence and early adulthood play a role. These factors contribute to the triggering of the disease and its individually varying course. With regard to the disease mechanisms, it is now proven that it is an autoimmune disease. In an autoimmune disease, the body’s immune system mistakenly targets the body’s own tissue. This may be caused by an incorrect reaction to infections with pathogens that resemble the body’s own structures. As a result, the body produces immune cells, primarily certain T lymphocytes, as well as antibodies against the body’s own myelin and nerve cells.
The complex genetic background means that first-degree relatives of a person affected by MS have a 20 to 40-fold increased risk of developing MS. With an incidence of around one in 1,000 people, this means a risk of two to four percent. The environmental factors also found, including vitamin D3, which is formed in the skin through exposure to sunlight, together with the genes occurring in certain population groups, mean that MS is found with greater frequency in both hemispheres of the earth with increasing distance from the equator.
Infections with certain viruses, in particular the Epstein Barr virus (EBV), which causes Pfeiffer’s glandular fever, as well as specific intestinal bacteria can contribute to the triggering and progression of MS according to current knowledge. There are indications of other possible triggers such as stress situations, hormonal fluctuations and individual medications, but these are not considered sufficiently certain.
Multiple sclerosis: frequency and age
Multiple sclerosis is the most common chronic disease of the central nervous system. It is the second most common neurological disease after epilepsy. Around 18,000 people with multiple sclerosis live in Switzerland.
Multiple sclerosis usually makes itself felt between the ages of 20 and 40. This makes MS the most common nerve disease in young adults. However, children and adolescents can also contract the disease. Women are affected about three times more often than men.
Multiple sclerosis symptoms
The symptoms of multiple sclerosis can manifest themselves in different ways. There are no specific signs of the disease that prove its presence. However, the occurrence of certain symptoms and the relapsing course in a young adult indicate MS.
Early symptoms and signs of the disease that occur particularly frequently in MS are:
- Sensory disturbances: Typical symptoms include numbness or tingling (formication) in the arms and legs, feelings of tension around the joints and hips, pain and reduced sensitivity, for example to temperature. The so-called neck flexion sign is also widespread. Those affected experience an electrifying, sudden shooting sensation along the spine when they bend their head forward.
- Visual disturbances: Many patients suffer from temporary visual disturbances – due to a temporarily inflamed optic nerve (so-called optic neuritis). Acute inflammation often causes pain in the eye area, which intensifies when the eye is moved. Blurred vision as if through a veil, impaired color vision or when reading small print, flashes of light or loss of visual field are other possible symptoms.
- Muscle paralysis: Multiple sclerosis is also characterized by reduced muscle strength and even paralysis, which can be accompanied by rapid fatigue when walking, tension and stiffness.
Multiple sclerosis can also cause numerous other symptoms, which can occur individually or in combination:
- If cranial nerves are affected, for example, facial paralysis(facial nerve palsy), pain (trigeminal neuralgia) or eye movement disorders (double vision) can occur, as can taste disorders and balance problems.
- Damage to the cerebellum usually results in speech disorders, unsteady gait, trembling hands or coordination disorders.
- Many of those affected develop bladder dysfunction. While a strong urge to urinate with involuntary loss of urine (incontinence) sometimes occurs at the beginning, involuntary urinary retention can also occur in the course of the disease.
- MS can also cause impaired defecation (usually constipation), impaired sexual function and impaired sweat secretion.
- Many sufferers also experience mood swings and depressive symptoms such as sadness, insomnia and listlessness.
The frequency of relapses, the respective symptoms and the progression of the disease vary greatly from person to person. Some sufferers have a (very) mild course and never acquire any significant disabilities, while a small number develop the disease aggressively and permanent signs of disability, such as walking difficulties, appear after just a few years. These courses have become rare due to the now much better treatment options. Before the introduction of effective treatments, a high percentage of those affected lost their ability to walk after 20-25 years, which is why it is still often assumed that the disease leads to the loss of the ability to walk, although this can now be prevented in most cases.
Diagnosis of multiple sclerosis
If multiple sclerosis is suspected, we will first ask you about your symptoms, including when they first occurred and how they manifest themselves.
Taking a medical history alone is not sufficient for a reliable diagnosis. We therefore carry out a neurological examination next. For example, we check the function of the cranial nerves and test sensation, reflexes and muscle strength. This allows the extent of the restrictions to be assessed.
An important part of the diagnosis is an examination of the so-called cerebrospinal fluid (CSF), which has a much higher diagnostic value than a blood test, and is obtained by means of a lumbar puncture. This is a simple and usually hardly painful examination. In the case of inflammatory changes in the brain and spinal cord, certain immune cells and antibodies are elevated in the cerebrospinal fluid. This can be proven on the basis of the sample obtained.
As this is also the case with other inflammatory diseases of the nervous system such as meningitis, other procedures are usually also used. Magnetic resonance imaging (MRI ) allows us to identify the inflammatory foci that are characteristic of the disease. Sometimes these foci are found by chance during an MRI scan for migraines or after a concussion, before the first symptoms appear. Additional examinations such as visual evoked potentials (VEP) and optical coherence tomography (OCT) measure the conduction velocity of the optic nerve and the damage to the retina of the eye in MS. Before a diagnosis of MS is made, other possible explanations (differential diagnoses) for the clinical symptoms are also ruled out.
Acute inflammation in the context of MS is known as an attack. This is the case when symptoms
- last for at least 24 hours,
- occurred at least 30 days after the start of the last episode and
- cannot be explained by fever (increased body temperature) or infection.
Multiple sclerosis: Important measures for those affected
Apart from avoiding individual risk factors, such as smoking, multiple sclerosis (MS) is not yet possible. As a sufferer, however, you can have a positive influence on the course of the disease by having it treated early and consistently and by taking certain measures yourself.
Nutrition
A healthy and balanced diet can help to favorably influence the course of the disease.
- Mediterranean diet: This diet is rich in fruit, vegetables, wholegrain products, fish and healthy fats such as olive oil. The consumption of red meat should be reduced.
- Vitamin D: Adequate vitamin D levels are important. Discuss with your doctor whether an appropriate supplement is necessary.
- Omega-3 fatty acids: These are found in fish oil and linseed and can have an anti-inflammatory effect.
Movement
Regular physical activity can help to maintain muscle strength, promote mobility and improve general well-being.
- Moderate exercise: Activities such as walking, swimming, yoga or tai chi can be helpful.
- Physiotherapy: An exercise program specially tailored to MS sufferers can help to maintain mobility, reduce muscle stiffness and improve coordination.
- Pacing: Make sure you structure your activities and plan breaks to avoid exhaustion.
Stress management
Stress can exacerbate MS symptoms. It is therefore important to learn techniques to manage stress effectively.
- Relaxation techniques: Methods such as meditation, breathing exercises and progressive muscle relaxation can help to reduce stress.
- Time management: Plan your day and set priorities to avoid being overwhelmed.
- Seek support: Sharing experiences with other sufferers, whether in self-help groups or by talking to friends and family, can provide emotional support.
Coping with everyday life
Adapting daily life and the living environment can help to maintain independence and make everyday life easier.
- Aids: Use technical aids and adaptations in the home to support your mobility and independence.
- Occupational therapy: This can help you learn techniques to make everyday tasks easier to manage.
- Workplace adjustments: Discuss with your employer ways of adapting your workplace to avoid overworking and maintain your productivity.
Stop smoking
Smoking can increase the risk of occurrence and have an unfavorable influence on the course of the disease. The clear recommendation is therefore to stop smoking.
Progression and prognosis of multiple sclerosis
Multiple sclerosis (MS) is a chronic disease, which means that it is usually permanent. However, early diagnosis and consistent treatment as well as the above-mentioned measures have a favorable effect on the disease, and it is now possible to prevent severe disabilities in most cases. It is therefore important, especially at the beginning, to consistently monitor the course of the disease and start suitable treatment at an early stage.
There are three main forms of multiple sclerosis:
- In relapsing-remitting multiple sclerosis, symptoms (“relapses”) occur suddenly within a few days. These often last for several days to weeks and usually disappear completely. The interval between episodes is very variable and can range from months to years.
- In the case of primary chronic progressive multiple sclerosis, the symptoms develop gradually but progress steadily. There are no acute relapses with this form of the disease.
- Secondary chronic progressive multiple sclerosis is characterized by the fact that the relapses that occur become less frequent as the disease progresses and eventually cease altogether. However, the disabilities caused by multiple sclerosis are steadily increasing.
As the course of multiple sclerosis varies greatly, a general prognosis is difficult. Some sufferers notice no deterioration or hardly any impairment for years between attacks and can lead a normal life. In rare cases, the disease can lead to severe disabilities as it progresses. In addition to the clinical course, imaging procedures(MRI) help to assess at an early stage how dynamically the disease is progressing and whether adjustments to the therapy are necessary.
It is important for you to know that the prognosis is often much better than expected.
Self-help groups
The exchange with people who are affected by the same disease can be a great support in coping with the disease. Advice on finding a suitable self-help group can be obtained in particular from the MS Society or the Self-help Zurich. Selbsthilfe Zürich and the University Hospital Zurich are cooperation partners in the national project “Health literacy thanks to self-help-friendly hospitals”.
Multiple sclerosis: Effective treatment
There is currently no cure for multiple sclerosis. However, there are numerous treatment options available to us. The aim is to reduce the extent of the inflammatory reactions, slow down the progression of the disease and alleviate the accompanying symptoms. It is important that the therapy is individually tailored to your case and the course of your illness. To do this, you should seek treatment at a center specializing in multiple sclerosis, such as the USZ. At the Neurology Clinic of the USZ, you will receive comprehensive advice on the most suitable therapy for you. In addition to all standard therapies, we are by far the largest MS center in Switzerland with experience in autologous hematopoietic stem cell transplantation for MS patients for whom standard medications are not effective enough. We will be happy to advise you if you are interested in this therapy. We also regularly offer new therapies as part of clinical trials. This helps to better understand the disease and further improve the prognosis for those affected in the future.
FAQ Multiple Sclerosis
Multiple sclerosis (MS) typically begins with non-specific symptoms that usually occur in episodes. Common early signs are visual disturbances, numbness or tingling in certain parts of the body, motor problems such as weakness or coordination problems, and fatigue.
The course of multiple sclerosis (MS) varies from person to person, typically with relapses followed by partial or complete recovery. In the long term, a gradual progression of symptoms can develop.
The exact causes of multiple sclerosis (MS) are not fully understood. It is assumed that a combination of genetic factors, environmental factors and the immune system play a role. Possible triggers include viral infections, vitamin D deficiency, smoking and certain genetic predispositions.
Multiple sclerosis (MS) is diagnosed through a combination of medical history, neurological examination, cerebrospinal fluid examination and imaging techniques such as MRI to identify inflammatory lesions in the central nervous system.
There are numerous medications available for the treatment of multiple sclerosis (MS), which are primarily aimed at preventing further inflammation. Symptomatic therapies for specific complaints, such as fatigue or pain, and rehabilitation measures such as physiotherapy to improve mobility are also important.
In multiple sclerosis (MS), there are no known specific blood values that are typically conspicuous. Diagnosis is based on clinical symptoms, neurological examinations, cerebrospinal fluid examination and imaging procedures such as MRI.
Multiple sclerosis (MS) is typically diagnosed between the ages of 20 and 40, with the average onset of symptoms often occurring around the age of 30.
The preliminary stage of multiple sclerosis (MS) is referred to as clinically isolated syndrome (CIS). This is a situation that shows typical features of inflammation in the central nervous system, but does not yet fulfill the full diagnostic criteria for MS. CIS can be the first sign of the risk of developing MS later in life.