What is lung cancer?
Lung cancer is a malignant tumor in the lungs. In medical terminology, this cancer is also known as lung carcinoma or bronchial carcinoma. Tumors in the lungs are malignant in the vast majority of cases – and only rarely benign. First of all, experts distinguish between lung cancer that has formed directly (primarily) in the lungs and lung metastases. In this case, the origin lies in another cancer in another organ. Breast or prostate cancer, for example, often metastasizes to the lungs.
Like every type of cancer, lung cancer develops from a cell in which the genetic material (the DNA) changes – the cell mutates. It can then divide and multiply unchecked. Doctors are aware of a number of risk factors that promote lung cancer. In addition to smoking, inhaling dust, chemicals and pollutants can also increase the risk of lung cancer.
Experts basically distinguish between two forms of lung cancer: the more common non-small cell lung cancer and the rarer small cell lung cancer, which grows faster and more aggressively. Lung cancer is particularly insidious because it only causes symptoms at a very late stage. By then it is often more advanced and has metastasized to other organs. The malignant tumor in the lung usually makes itself felt through a persistent cough and shortness of breath, which is often interpreted as a harmless respiratory infection or bronchitis.
Lung cancer can be successfully treated, usually with surgery, radiotherapy and drug therapy, which can include chemotherapy, immunotherapy or drugs that target specific characteristics of the tumor (targeted therapy).
As with any type of cancer, the earlier we diagnose and treat lung cancer, the better the chances of survival.
Lung cancer – frequency and age
Alongside prostate, breast and colon cancer, lung cancer is one of the most common types of cancer. In Switzerland, the third most common cancer diagnosis is „lung cancer“, but it is also the most common cancer leading to death Every year, around 2,600 men and around 1,700 women in Switzerland are diagnosed with lung cancer. Men are (still) in the majority. But in many countries, women are catching up because they either used to smoke or are still smokers. Almost all of them are over 50 years old at the time of diagnosis. Many do not survive the first five years because the lung cancer is already well advanced at the time of diagnosis.
Lung and Thoracic Oncology Center
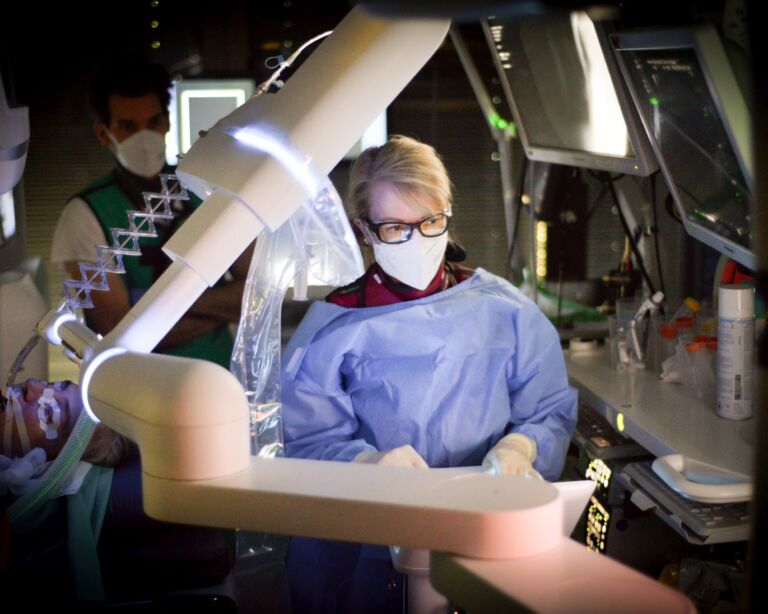
At the USZ, numerous specialist departments have joined forces to form a lung and thoracic oncology center. The center is certified according to the guidelines of the German Cancer Society (DKG). A team of experts specializing in the medical treatment of lung cancer works closely together here for the benefit of our patients. At DKG-certified centers, patients are treated according to strict quality criteria and, according to current studies, have a better chance of survival on average.
Lung cancer: causes and risk factors
The development of cancer always begins with a change in the genetic material of a cell – it mutates. It can then divide unchecked, multiply and form a tumor. Lung cancer usually originates in the mucosal cells of the bronchial tubes. Harmful substances that enter the lungs with the air we breathe act on these cells and change them. However, cancer researchers now believe that there is no „one“ cause of cancer, but that several factors must interact in its development.
Lung cancer: Smoking is the main cause
The most important – but not the only – cause of lung cancer is smoking. Tobacco smoke contains carcinogenic substances. The decisive factor here is how long and how much someone has smoked. Doctors speak of so-called „pack years“. In many cases, lung cancer develops very slowly: on average, it takes 20 years from the start of smoking for the cancer to develop. The more and longer someone has smoked, the higher their risk of lung cancer. Tobacco smoke from cigars and pipes is also carcinogenic, although it causes less lung cancer and more mouth, throat and larynx cancer.
Passive smoking is also considered a risk factor for bronchial carcinoma. As a result, smoking in public buildings, facilities and transportation is now prohibited by law in most countries. It is still unclear whether and to what extent e-cigarettes contribute to the risk of lung cancer. It is worth quitting smoking at any age. The risk decreases again if you become and remain smoke-free.
However, it should not be forgotten that non-smokers can also develop lung cancer.
In addition to smoking, the following factors are involved in the development of lung cancer:
- Pollutants that most people come into contact with at work: Examples include asbestos, arsenic, chromium and nickel compounds, quartz dusts and polycyclic aromatic hydrocarbons (PAHs)
- Radioactive radiation and X-rays, for example from flights or medical examinations
- Radon – a radioactive noble gas that rises from the ground and can accumulate in living and working spaces. In some regions, it is increasingly released from the soil.
- Particulate matter – tiny particles released into the air by car traffic, industry and households
- Diesel soot: pollutants from diesel engines
- Previous lung diseases, for example infections such as tuberculosis or injuries to the lungs where scars have formed
Researchers are also discussing a number of other factors as causes of lung cancer, but their role in the development of the disease has not yet been clearly established. Examples are:
- Infections with HP viruses (HPV) or HI viruses (HIV)
- Hereditary predisposition (genes): If a parent has lung cancer, children have a two to three times higher risk of developing the disease themselves. This correlation is particularly true if the parent fell ill at a young age.
- Diet: It is not yet entirely clear how important diet is for the risk of lung cancer. However, results from studies suggest that eating a lot of fruit in particular can protect against lung cancer.
- Lack of exercise appears to contribute to the risk of lung cancer.
Symptoms: Lung cancer often shows up late
Lung cancer hardly causes any symptoms for a long time. And if so, the bronchial carcinoma is often already very advanced. In addition, the symptoms are relatively unspecific and can also occur in many other diseases. Most people associate their cough less with lung cancer and more with a respiratory infection or bronchitis. They do not seek medical advice at first.
Symptoms of lung cancer can include
- persistent cough with sputum that does not subside even after several weeks
- Hemoptysis as a special form, should always be clarified
- in smokers who have been smoking for years: chronic smoker’s cough that changes or worsens
- Shortness of breath,
- Permanent pain in the chest
Always consult your doctor if you notice a persistent cough or other symptoms. This is especially true if you have been smoking for years. The earlier lung cancer is found, the easier it is to treat and the better the chances of survival.
Diagnosis of lung cancer
A lung cancer diagnosis always begins with a discussion with us about the patient’s medical history (anamnesis). These questions are important, for example:
- What symptoms do you have – for example, coughing, shortness of breath?
- When did you first notice the symptoms?
- How pronounced are the symptoms and have they worsened recently?
- Do you smoke? If yes: How long have you been smoking and how much?
- Are you frequently exposed to harmful substances at work or at home?
- Do you have any known diseases?
- Are there any illnesses in your family?
- Are you taking any medications? If yes: Which and since when?
Your answers will give us some initial clues as to what could be the cause of your symptoms. This is usually followed by a physical examination. This includes listening to the lungs with a stethoscope.
Suspected lung cancer – these tests provide information
This is followed by further examinations to establish a diagnosis of lung cancer or to rule out the disease. The most important are:
- X-ray examination of the thorax: This is often the first examination performed in the event of symptoms. Serves to differentiate from other pathologies
- Computed tomography (CT): CT allows the airways and changes in the lung parenchyma to be visualized. Is the method of choice for confirming a tumor. It is also used to determine the extent and staging of the disease.
- Magnetic resonance imaging (MRI ): Is increasingly used in the clinic, as it helps to better delineate the boundaries of the tumor in relation to other organs, e.g. when growing into the thoracic wall.
- Lung endoscopy (bronchoscopy): We examine the airways with a bronchoscope. We advance a thin, flexible tube into the lungs via the windpipe, which is equipped with a small camera. This examination is always carried out during artificial sleep (sedation or anesthesia).
- Tissue sample (biopsy): As part of the bronchoscopy, we can take a tissue sample from the suspicious areas of the lung at the same time. The cells are then examined under a microscope by a pathologist in the laboratory. You can see whether they are benign or malignant. This makes it possible to diagnose lung cancer with certainty. Another way to obtain tissue is in the form of a thoracoscopy (see below).
Diagnosis of lung cancer – further examinations to determine the extent of the tumor
If the diagnosis of lung cancer is confirmed, further examinations will follow. The size of the tumor is examined and how far it has already spread, i.e. what stage it is in. Malignant tumors are often no longer limited to the lungs at the time of diagnosis. Lung cancer often spreads to other organs and forms metastases there – such as in the liver, bones, adrenal glands and brain.
The following examinations show where the tumor is located and what stage it is in:
- Positron emission tomography/CT(PET/CT): PET/CT shows particularly metabolically active areas, for example metastases. We usually use the radioactively labeled sugar „18F-FDG“ as the radioactive substance.
- Magnetic resonance imaging (MRI = magnetic resonance imaging) of the brain: Radiologists work with strong magnetic fields and create sectional images. The images show whether metastases are present in the brain.
- Bronchoscopy with endobronchial ultrasound (EBUS): This examination is often performed in the same session as the bronchoscopy described above for diagnostic purposes. To examine the lymph nodes, a miniature ultrasound probe is also inserted into the airways together with the bronchoscope.
- Thoracoscopy: Sometimes fluid accumulates in the pleural cavity and we take a sample to examine it for cancer cells. On this occasion, samples can also be taken from the tumor or the pleura.
- Mediastinoscopy: A procedure in which we insert a flexible instrument (endoscope) into the space between the two lungs. This allows lymph nodes to be removed and examined for cancer cells in pathology.
- Blood test: The blood values generally show how well the organs are functioning.
- Genetic test: Lung cancer, like all other types of cancer, is caused by acquired genetic changes. An increasing number of these changes enable targeted drug therapy.
- As a rule, functional diagnostics of the lungs are carried out, such as spirometry. It shows how efficient the lungs are.
What type of lung cancer is there?
We distinguish between two types of lung cancer, which have different frequencies and different dangers. Treatment also depends largely on this.
- Non-small cell l ung cancer (NSCLC): The majority of people with lung cancer (around 90 percent) suffer from non-small cell lung cancer. The tumor cells appear larger under the microscope. Non-small cell lung cancer grows relatively slowly, often in limited areas of the lung and also forms metastases less quickly. In the early stages, NSCLC can often be removed by surgery.
- Small cell l ung cancer (SCLC): This type of lung cancer is rarer and more aggressive. Small cell lung cancer grows quickly and spreads to other organs at an early stage. The prognosis is therefore less favorable. We usually combine several therapies to keep lung cancer at bay.
Lung cancer stages: TNM classification
We classify lung cancer into different stages. The higher the stage, the more advanced the cancer and the less favorable the prognosis. The so-called TNM classification is internationally recognized:
- T (tumor): How large is the tumor and how far has it spread? (T1 to T4)
- N (node = lymph node): Are there cancer cells in the lymph nodes? (N0 to N3)
- M (metastases): Are metastases present in other organs? (M0 = no metastases and M1 = there are metastases)
Based on the TNM classification, lung cancer is categorized into stages 1 to 4. The higher the number, the more advanced the lung cancer. The treatment also depends on this.
Second opinion for lung cancer
When a cancer diagnosis is made, a second medical opinion is an important decision-making tool. The Comprehensive Cancer Center Zurich supports you with a professional expert opinion. They receive a thorough analysis of the situation as well as personal advice and quick answers to their questions.
Lung cancer: prevention, early detection, prognosis
The main cause of lung cancer is smoking. You can therefore effectively prevent smoking by not starting in the first place. And if you smoke, try to stop – it’s worth it at any age. Seek professional support if you cannot quit cigarettes or other smoking products on your own. Further tips on prevention:
- Do not smoke passively with others.
- Some people try to switch to e-cigarettes. Although they are considered less harmful, the health effects of vaping are not yet entirely clear.
- Make sure you take adequate protective measures at your workplace if you are exposed to harmful substances.
- Eat healthily, preferably lots of fruit and vegetables – your whole body will benefit from this.
- Move a lot in everyday life and do sports.
- If radon is leaking from the ground where you live – pay attention to the floors in the building and have them remediated if necessary.
Early detection measures using computer tomography in heavy smokers can be life-saving; their introduction in Switzerland is currently being reviewed for lung cancer is currently being tested as part of a pilot project at the USZ. The following therefore applies in general: always consult your doctor promptly if you experience symptoms such as coughing or shortness of breath.
Progression and prognosis of lung cancer
The course and prognosis of lung cancer depend on the type, stage, spread and aggressiveness. Life expectancy and chances of recovery are generally higher with non-small cell lung cancer than with small cell lung cancer. Women also often survive longer than men. Your age and general state of health also play a role. Compared to other types of cancer, however, the prognosis for lung cancer is less favorable. Generally speaking, the earlier we find the lung cancer, the better the chances of treatment and recovery. This also increases life expectancy. However, it is also true that the prognosis is often not as good as for other types of cancer.
Self-help groups
The exchange with people who are affected by the same disease can be a great support in coping with the disease. Advice on finding a suitable self-help group is available from Selbsthilfe Zürich. Self-Help Zurich and the University Hospital Zurich are cooperation partners in the national project „Health literacy thanks to self-help-friendly hospitals“.
Lung cancer: treatment with several therapies
The treatment of lung cancer always depends on the type, stage and spread of the tumor. These factors also determine which therapies we choose. Small cell lung cancer, for example, responds to different treatments than non-small cell lung cancer. We usually combine several treatments to increase their effectiveness. In addition, specialists from several disciplines are always involved in the treatment of lung cancer. These include: oncology, lung surgery, pathology, radiation oncology, psycho-oncology and lung specialists. There is also the possibility of accompanying complementary medical treatment.