Overview: What is endometriosis?
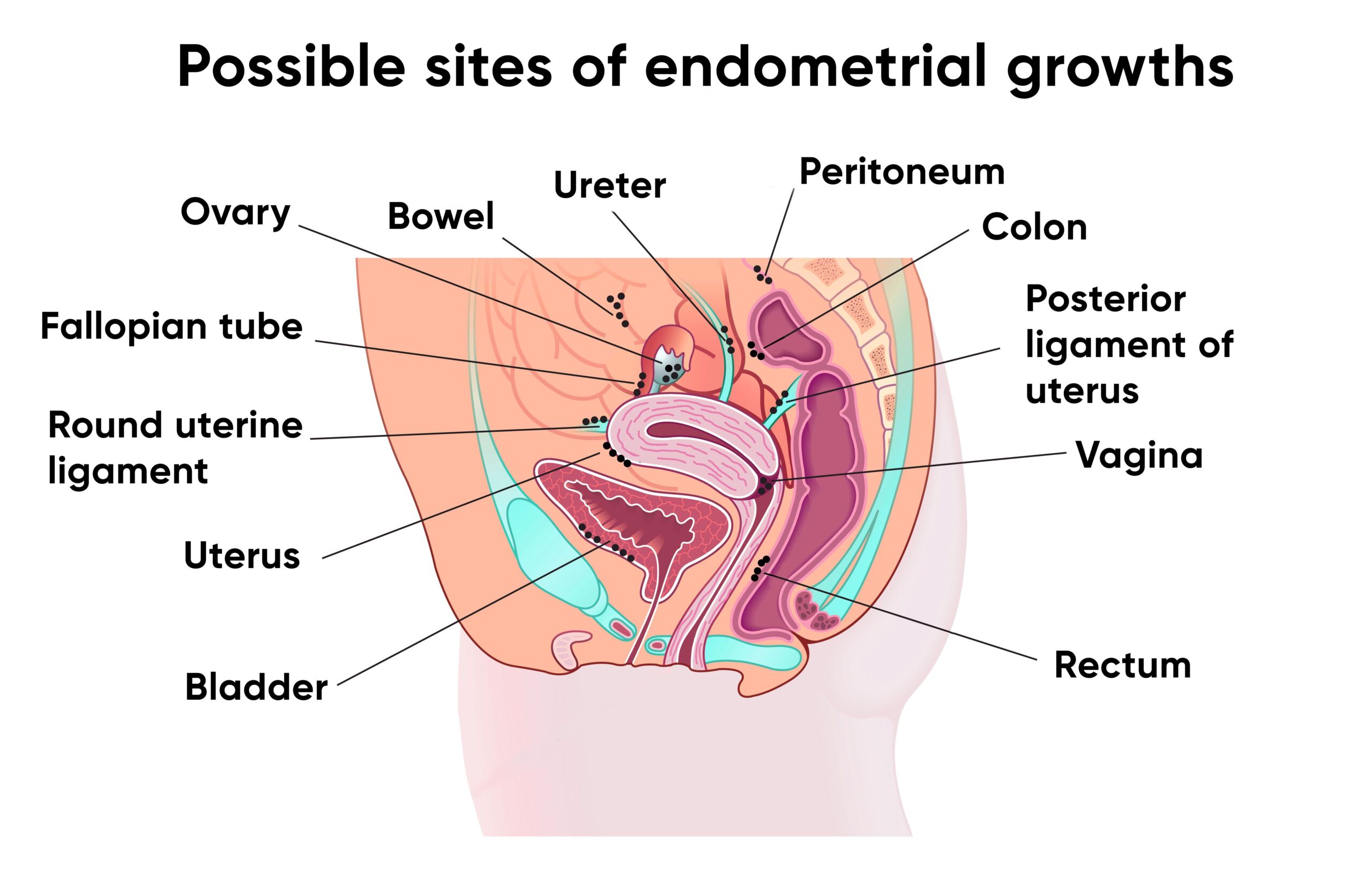
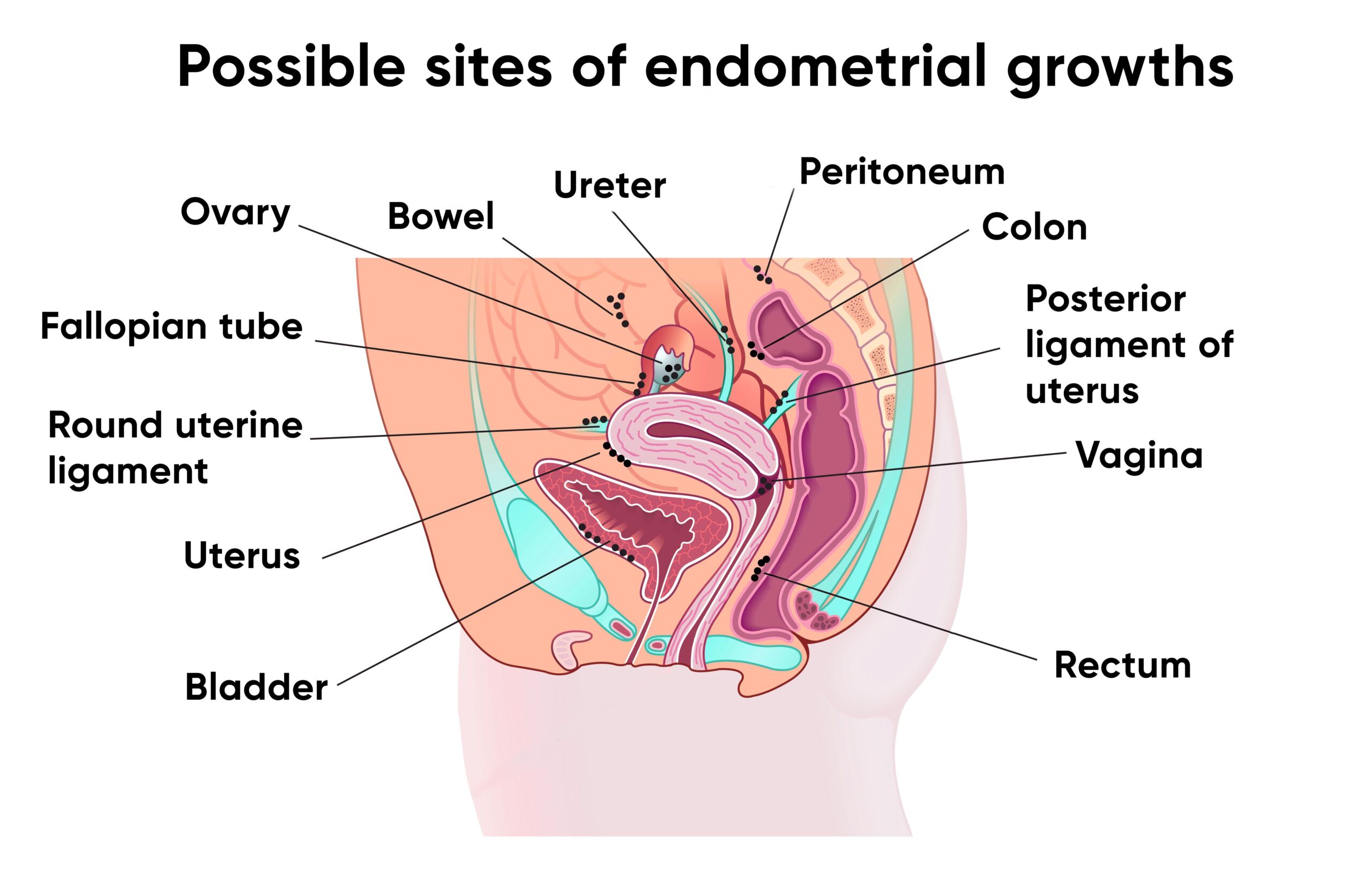
We refer to the endometrium as the lining of the uterus. Endometriosis is the term used to describe the abnormal presence of the uterine lining outside the uterine cavity in the pelvic area, but in rare cases also in various other places inside and outside the entire abdominal cavity.
Organs such as the bowel, bladder or even the lungs can also be affected.
Endometriosis presents itself in various forms.
Endometriosis on the peritoneum usually corresponds to small foci resembling a birthmark on the skin.
So-called endometriomas or “chocolate cysts” often form on the ovary.
So-called deep infiltrating endometriosis describes lumps that can grow into the uterine retaining ligaments, bowel or bladder.
We speak of adenomyosis when endometrium-like tissue occurs in the muscle wall of the uterus.
What all these forms have in common is that they are stimulated by the sex hormones of the menstrual cycle and cause a local inflammatory reaction.
As a result, affected individuals suffer from pain in this area due to the irritated nerves caused by the inflammation. Women affected often experience severe pain during menstruation in particular.
Later on, this pain can also occur long before menstruation or completely independently of it – this is referred to as chronic pain.
In addition, many affected people have difficulty getting pregnant.
Endometriosis: frequency and age
It is not uncommon for patients to suffer for more than five years before they are diagnosed with endometriosis. Nevertheless, many women live with this problem without knowing about it. It is estimated that around six to ten percent of all women of childbearing age suffer from endometriosis. In Switzerland, this means around 190,000 to 280,000 women. About one in four women who do not become pregnant spontaneously suffers from endometriosis.
The symptoms may already be present at a young age with the onset of menstruation, or may only increase over the years.
After the onset of the menopause, the symptoms usually decrease significantly or disappear completely.
Endometriosis: causes and risk factors
Why in some women the mucosa from the uterus settles within the pelvis and abdomen is still unclear in detail. Accordingly, the development of endometriosis cannot be prevented. The disease occurs more frequently in some families than in others. If the mother suffered from endometriosis, the daughter has a six times higher risk of also suffering from endometriosis during her reproductive years. Despite this familial clustering, no single endometriosis gene has yet been found.
Environmental influences – in the womb, during the neonatal period – and nutritional factors also appear to play a role.
A possible explanation for the development of endometriosis is so-called “retrograde menstruation”: Instead of the menstrual blood flowing completely through the cervix into the vagina, part of the menstrual blood enters the abdominal cavity through the fallopian tubes together with exfoliated endometrial cells. The inflammation caused by this leads to severe pain by irritating the nerves. This theory can explain the most common sites, which are affected with endometriosis in the abdomen. There are also cases in which the endometrial cells enter the muscle layers of the uterine wall through tiny openings/micro-injuries and can also grow there. In this case we speak of adenomyosis, a close relative of endometriosis.
In rare cases, endometriosis can also affect other organs, such as the liver, lungs or even the brain, which cannot be explained by the theory of retrograde menstruation. In these cases, endometriosis appears to develop directly in the affected organs, in that so-called cells of origin mistakenly develop into endometriosis cells instead of, for example, liver cells in the case of the liver.
Symptoms of endometriosis
Very often, women tell of severe pain during menses with frequent use of painkillers and sick leave. If this pain has only developed over the years (so-called “secondary dysmenorrhea”), endometriosis is most likely present.
The following symptoms are still possible:
- Pain during sexual intercourse
- Feeling of bloating during menstruation
- Abdominal pain regardless of the timing of menstruation
- Back pain
- disturbed menstrual cycle (intermittent bleeding, prolonged or heavier bleeding)
- noticeable fatigue and exhaustion
- increased susceptibility to infections, especially during menstruation
- Pain when urinating or blood in the urine
- Pain during bowel movements or blood in the stool
Where the pain occurs depends on where the mucosal tissue has settled. In the vast majority of cases, these are distributed in the pelvic cavity on the peritoneum (especially in the Douglas space) and lead to severe pain during the period. If endometriosis lesions are found in the vaginal area, they can cause pain during sexual intercourse by touching.
If the focus of the disease is on the bladder, it becomes irritated and one feels frequent urge to urinate. In rare cases, when such a focus grows deep into the urinary bladder, blood may even be found in the urine. If the bowel is affected, affected women report severe pain during defecation and may even have blood in their stool if the bowel is breached. It is typical for endometriosis if the symptoms mentioned occur depending on the menstrual cycle. This cycle dependency can also be absent in long-term courses. The nerves that transmit the pain signals from these foci are then permanently “irritated”. Endometriosis on the ovary – so-called endometriomas or chocolate cysts – rarely cause pain on their own, but are often associated with the simultaneous occurrence of a severe form of endometriosis called “deep infiltrating endometriosis”.
When the endometriosis focus is in the muscular layer of the uterus, menstruation usually comes in a strikingly heavy and prolonged manner.
Register for consultation
Infertility due to endometriosis
Endometriosis lesions can directly adhere to the fallopian tubes or destroy ovarian tissue, making it difficult or impossible to transport the egg to the uterus and fertilize it in the fallopian tubes. However, it is much more common that endometriosis seems to indirectly hinder the process of fertilization and implantation in the uterine cavity due to the regional inflammatory situation. This is why many women with endometriosis have difficulties getting pregnant. However, if endometriosis is detected, help can be provided either by surgery or direct treatment by a fertility specialist.
Pregnancy despite endometriosis
Once all endometriosis lesions have been removed, pregnancy is possible in many cases, provided the fallopian tubes are not blocked. In some other cases, however, reproductive treatment such as in-vitro fertilization, i.e. fertilization of the egg outside the body, is necessary. The fertilized egg is then placed directly into the uterus.
Endometriosis: diagnosis with us
The basis of the diagnosis of endometriosis is the assessment of the exact symptoms. If you can describe to us in as much detail as possible when, where and in what situation the pain occurs, this will help us to make a diagnosis. An unfulfilled desire to have children is just as much a part of it. This is usually followed by a gynecological examination incl. Palpation examination.
Ultrasound examinations are particularly important, as certain forms of endometriosis (e.g. so-called
endometriomas/chocolate cysts on the ovary) can be diagnosed directly by ultrasound. Experienced examiners can also detect adhesions, adhesions of the organs and endometriosis nodes (deep infiltrating endometriosis).
If deep infiltrating endometriosis is suspected, magnetic resonance imaging (MRI) is also carried out in certain cases. It allows a more precise view of the localization of the endometriosis nodes and can also show areas outside the pelvis.
Rarely, blood may be present in the stool with this form of endometriosis. In this case, we recommend a colonoscopy.
In the most common form, known as peritoneal endometriosis, there are only very small or flat endometriosis lesions in the abdominal cavity. This form cannot currently be visualized by ultrasound or MRI.
These cases can only be made visible with a small operation – a laparoscopy: A tiny camera is inserted into the abdominal cavity through a small incision in the navel and the peritoneum and pelvic organs are viewed with a slight magnification of the camera image so that even millimeter-sized endometriosis lesions can be detected. If the suspicion is confirmed, we can also remove the herd directly. But don’t worry – surgery is only necessary in certain cases of peritoneal endometriosis.
Taking hormonal therapy (a special contraceptive pill) on a trial basis can often be helpful: if the pain disappears while taking the pill, there is a high probability that endometriosis is present. For most women, this method helps against pelvic pain.
In unclear cases or those in which other diseases are also a possible cause of the symptoms, it is also possible to clarify the presence of endometriosis using a saliva test.
Endometriosis: prevention, early detection, prognosis
You cannot prevent endometriosis. However, you should consult a doctor in case of prolonged menstrual irregularities and especially if you experience severe pain during your period.
Endometriosis consultation
Do you have any questions or would you like clarification? Register and receive further information in a personal consultation.
Treatment details
What endometriosis means for affected women in everyday life can be completely independent of the size and location of the proliferating mucous membrane. Some women do not notice anything, others suffer from the most severe pain.
Endometriosis is treatable but not curable. After surgical removal of the endometriosis, the pain usually subsides, but can reappear as soon as the endometriosis starts to grow again. Hormone therapy is therefore important as a preventive but also pain-relieving measure. The treatment of endometriosis is long and often very stressful for women.
Endometriosis does not generally increase the risk of developing cancer. For certain, rare cancers of the ovary, however, endometriosis appears to be clustered with it.
Self-help groups
The exchange with people who are affected by the same disease can be a great support in coping with the disease. Advice on finding a suitable self-help group can be obtained from the Swiss endometriosis association Endo-Help or from Selbsthilfe Zürich. Selbsthilfe Zürich and the University Hospital Zurich are cooperation partners in the national project “Health literacy thanks to self-help-friendly hospitals”.
Treatment: with hormones or surgery
There is no way to cure endometriosis yet. Medication and surgery are available to combat the symptoms:
- Anti-inflammatory painkillers
- Hormonal therapy
- Surgery
- alternative methods of pain relief
Which of these methods is chosen depends, on the one hand, on whether the woman concerned wants to have children or whether family planning has already been completed. Second, treatment depends on exactly where the endometriosis is located and how large it is. If a woman has neither complaints nor a desire to have children, no treatment is necessary. At the USZ, we work with you to create a treatment plan for you and your individual situation. Our Endometriosis Nurse will accompany you throughout your treatment.