Abdominal pain and diarrhea are common symptoms. The end section of the small intestine, the so-called “terminal ileum”, is most frequently inflamed. This is why the disease used to be called “ileitis terminalis”. Although chronic inflammatory bowel disease cannot be cured, the vast majority of cases can be controlled with the right treatment.
What is Crohn's disease?
Crohn’s disease is a chronic inflammatory bowel disease that often progresses in episodes and frequently recurs. This means that periods without symptoms alternate with periods of illness. The disease is chronic – and therefore usually a lifelong companion. However, it can usually be treated well so that normal everyday life is possible.
Crohn’s disease owes its name to the US gastroenterologist Burrill Bernhard Crohn, who first described it. It has many other names, for example Crohn’s disease, enteritis regionalis, enterocolitis regionalis, ileitis terminalis or Crohn’s disease.
Crohn’s disease – the characteristics
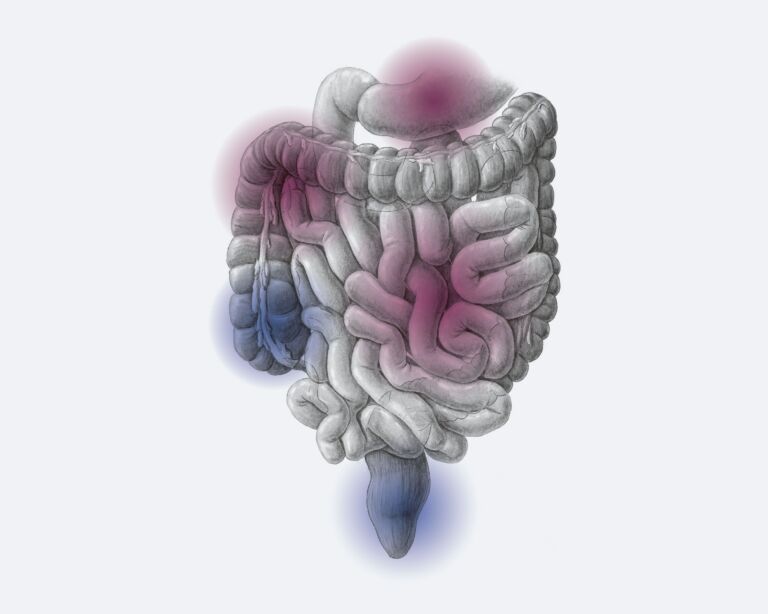
The inflammation can affect the entire digestive tract, from the mouth to the anus. However, they most frequently occur at the point where the small intestine joins the large intestine. This last area of the small intestine is called the “terminal ileum”. In addition, the inflammation can affect not only the uppermost layer of the mucous membrane, but all layers of the intestinal wall.
A further characteristic of Crohn’s disease is that the inflammation does not spread continuously throughout the intestine, but rather the inflammatory foci develop at several, non-contiguous points in the intestine. In between are healthy intestinal sections. Doctors refer to this pattern of infestation as segmental, discontinuous infestation.
Differences in ulcerative colitis
The situation is different with the very similar bowel disease ulcerative colitis:
- The inflammation usually only affects the large intestine.
- Only the uppermost layer of the intestinal wall, the intestinal mucosa, becomes inflamed.
- The inflammation begins in the rectum and spreads from there.
- The foci of inflammation are connected and are not interrupted by healthy sections of the intestine.
- Bloody, slimy diarrhea is common.
Among other forms of intestinal inflammation, doctors summarize both clinical pictures under the term chronic inflammatory bowel disease (IBD).
Crohn’s disease – frequency and age
Chronic inflammatory bowel disease (IBD) is one of the most common diseases in Switzerland: Around one in 350 people suffer from it. This means that more than 25,000 people are affected by IBD. Men and women fall ill about equally often.
In principle, Crohn’s disease can affect people of all ages. The intestinal disease usually first appears in adolescents and young adults, between the ages of 15 and 34.
Crohn's disease: causes and risk factors
The causes of Crohn’s disease are still largely unknown. Researchers do not yet know exactly what triggers ulcerative colitis either. However, there is probably not “one” cause, but several factors must interact in the development. However, one thing is clear: Crohn’s disease is not an infectious disease and is therefore not contagious to others.
Doctors are aware of a number of risk factors associated with Crohn’s disease.
Examples of risk factors
- Genes: Hereditary factors appear to play a role in Crohn’s disease. Chronic intestinal inflammation is more common in some families. In addition, certain genetic changes can be detected in some affected people, for example an altered NOD2/CARD15 gene. However, there are over 150 other known genetic risk factors that can increase the risk of Crohn’s disease. The genes in turn influence the cooperation between intestinal bacteria and the intestine. They account for around 30 to 40 percent of the maximum risk of disease.
- Environmental factors: The accumulation of the disease in the western world over the last 50 years and the increase in recent years, for example in China or Indonesia, suggest that the “western lifestyle” plays a role in the development and progression of the disease. Environmental factors are therefore major triggers for the disease and for inflammatory flare-ups.
- Altered intestinal flora: The human intestine is home to millions of bacteria and other germs of all kinds. The entirety of all microbes in the gut is called the “microbiome”. Healthy intestinal flora is important for normal intestinal function. The latest research suggests that a disturbed intestinal flora may not only be associated with Crohn’s disease, but also with many other diseases.
- Impaired intestinal barrier: The barrier of the intestinal mucosa probably does not function properly in Crohn’s disease. It normally ensures that no bacteria from the intestine can penetrate the intestinal wall. If they succeed, this is followed by strong immune reactions in the intestinal wall. This is because the body classifies the bacteria as “pathogens”, even if they are not actually dangerous. Intestinal inflammation occurs because the body activates various inflammatory cells to defend itself against danger.
Researchers have also identified several other risk factors for Crohn’s disease. These include, for example, smoking or treatment with antibiotics during adolescence.
Psychological factors do not appear to play a role as causes of Crohn’s disease. However, emotional stress or conflicts can influence the course of chronic inflammatory bowel disease. They can either trigger new relapses or exacerbate existing ones.
Symptoms: Crohn's disease is multifaceted
Crohn’s disease can cause a wide variety of symptoms, which primarily affect the gastrointestinal tract. However, the symptoms can also occur outside the bowel and extend to other areas of the body. However, not every patient develops all symptoms to the same extent. The chronic inflammatory bowel disease ulcerative colitis also causes similar symptoms. These symptoms are common in Crohn’s disease:
- Abdominal pain, often as abdominal cramps in the right lower abdomen, but also in other regions of the abdomen
- Diarrhea: The stool is liquid and watery, sometimes containing blood or mucus. Some people with Crohn’s disease also suffer from a food intolerance or food allergy. This can make the diarrhea and abdominal pain even worse.
- Loss of appetite
- Weight loss: Due to the diarrhea, the body loses a lot of protein and therefore energy and weight.
- Tiredness, fatigue, reduced physical performance
- General feeling of illness
- Fever
- Anemia due to a lack of iron or vitamin B12, other deficiency symptoms.
Other symptoms – depending on the activity of the disease
They affect a wide variety of organs:
- Joint problems
- Kidney stones
- Eye inflammation: Sclera or anterior part of the middle part of the eye
- Skin problems, for example aphthae – these are inflammatory changes to the mucous membranes in the mouth
- Liver: Chronically inflamed bile ducts or liver inflammation (autoimmune hepatitis, overlap syndrome)
- Bones: Low bone density (osteopenia) or bone loss (osteoporosis)
- Psyche, for example depression
Highly specialized, interdisciplinary team
At the USZ, patients with Crohn’s disease are cared for by a highly specialized, interdisciplinary team of gastroenterologists and surgeons. We discuss complex cases in a joint consultation, in which individual treatment plans are determined and the indications for complex operations are carefully examined.
Crohn's disease: how we proceed with the diagnosis
When diagnosing Crohn’s disease, we always start with your medical history. The following questions, for example, are interesting for him to gain initial clues:
- What are your symptoms?
- When did you first discover this?
- How pronounced are the symptoms?
- Do you have any other known illnesses?
- Do you have a family history of chronic inflammatory bowel disease?
- Are you taking any medications? If yes: Which ones?
- Have you taken any medication in the past and what kind?
This is followed by a physical examination during which we palpate the abdomen. For example, the size and position of organs can be determined.
We also use imaging examinations and various laboratory tests to diagnose Crohn’s disease.
- Blood test: For example, the inflammation values (e.g. C-reactive protein, CRP), red blood cells (anemia) or certain vitamins and minerals (malnutrition) are determined.
- Stool sample: Examination for bacteria to rule out intestinal inflammation due to pathogens. In addition, the calprotectin level can be determined from the stool. Calprotectin is a protein found in inflammatory cells. When these migrate into the intestinal wall and die and decay, they release the calprotectin into the stool. The severity and extent of the intestinal inflammation can be inferred from the level of calprotectin. The value is therefore also very suitable for assessing the response to therapy and the risk of a renewed inflammatory flare-up.
- Ultrasound (sonography): We examine the abdominal cavity using a transducer that emits and receives sound waves. Adhesions or fistulas on organs can also be detected. The Department of Gastroenterology is considered a world expert center for colon ultrasound.
- Colonoscopy (colonoscopy): The bowel is examined using an endoscope (flexible tube with camera). We can visualize changes and inflammations in the intestine, but at the same time take tissue samples (biopsies) from conspicuous areas. The cells are then examined by a pathologist in the laboratory.
- Magnetic resonance imaging (MRI, magnetic resonance imaging): This method works with strong magnetic fields. The body is imaged “slice by slice”, providing radiologists with high-quality cross-sectional images. MRI images use a contrast agent to show which areas of the intestine are inflamed and to what extent.
Highly specialized, interdisciplinary team
If only the large intestine is inflamed, even experienced doctors cannot always easily distinguish between Crohn’s disease and ulcerative colitis. Sometimes only the course of the disease reveals which of the two chronic inflammatory bowel diseases is actually involved. Sometimes it is not possible to make a clear distinction between the two forms over a longer period of time, which is then referred to as IBDu (IBD unclassified)
Crohn's disease: prevention, early detection, prognosis
The causes of Crohn’s disease are still largely unclear. There is therefore no way to prevent chronic intestinal inflammation (primary prevention). If you have Crohn’s disease, it is important to prevent a return of the disease in the form of new flare-ups – so-called secondary prevention. Giving up smoking seems to have a positive effect here.
Early detection plays a role in Crohn’s disease because those affected have an increased risk of bowel cancer. And in general: Crohn’s disease that is detected early can also be treated better. This reduces the risk of health consequences and complications.
Progression and prognosis of Crohn’s disease
Crohn’s disease is one of the chronic diseases that accompany you throughout your life. There is currently no cure for Crohn’s disease. But the bowel disease can be treated well, so that a normal everyday life with a good quality of life is often possible. Crohn’s disease progresses in episodes: phases of the disease alternate with periods without symptoms.
However, you can positively influence the course of the disease to a certain extent: seek psychological support or learn a relaxation technique such as Jacobson’s progressive muscle relaxation or autogenic training.
The course of Crohn’s disease varies greatly from person to person. It is therefore not possible to make any general statements about the forecast. Most people are able to cope with their everyday lives and do their jobs. Life expectancy is also hardly limited. However, it should be noted that the risk of bowel cancer is higher in people with Crohn’s disease than in people without the disease.
Complications of Crohn’s disease
Crohn’s disease can lead to various complications – either from the disease itself or from the various treatments.
Self-help groups
The exchange with people who are affected by the same disease can be a great support in coping with the disease. Advice on finding a suitable self-help group is available from Selbsthilfe Zürich. Self-Help Zurich and the University Hospital Zurich are cooperation partners in the national project “Health literacy thanks to self-help-friendly hospitals”.
- Fistulas: These are tube-like connections between organs and tissues that are unnatural and should not occur there. You can recognize that such fistulas have formed by the following signs, for example: Soiled underwear, stool in the urine or stool discharge via the vagina. Close collaboration between gastroenterology and surgery is particularly important for more complex fistulas, which is why a specialized interdisciplinary fistula consultation was established at the University Hospital several years ago.
- Abscesses: The tissue becomes inflamed and pus accumulates, which is very painful. Abscesses form preferentially in the anal area.
- Adhesive intestinal loops: Due to inflammation, parts of the intestine can stick together and form (benign) tumors. Conglomerate tumor is the medical term for this. The adhesions can often be felt from the outside.
- Intestinal bleeding: They are the result of a damaged and strained intestine. We can often stop the bleeding during a colonoscopy. Blood transfusions can compensate for blood loss.
- Intestinal obstruction: The causes are scars in the intestine or swellings that have formed due to inflammation. Surgery is usually necessary. However, if there is swelling in the bowel, the bowel contents can sometimes be suctioned out and the operation is unnecessary.
- Intestinal rupture: This complication of Crohn’s disease is highly feared, life-threatening and an acute emergency. Due to the inflammation, the intestine is damaged and can break through. We need to operate immediately.
Other possible complications, although these occur less frequently:
- Kidney stones
- Joint inflammation and joint pain
- Eye inflammation
- Inflammation of the bile ducts, inflammation of the liver
- Skin changes, often as painful skin nodules (erythema nodosum)
- Reduced bone density (osteopenia) and bone loss (osteoporosis)
Crohn's disease: treatment is based on several pillars
There are several treatment options for Crohn’s disease, which we often use in combination. This increases their effectiveness and impact. The aim of treatment is always to alleviate symptoms, reduce the number of relapses, extend the time between relapses and prevent complications.