What are the functions of the intestine?
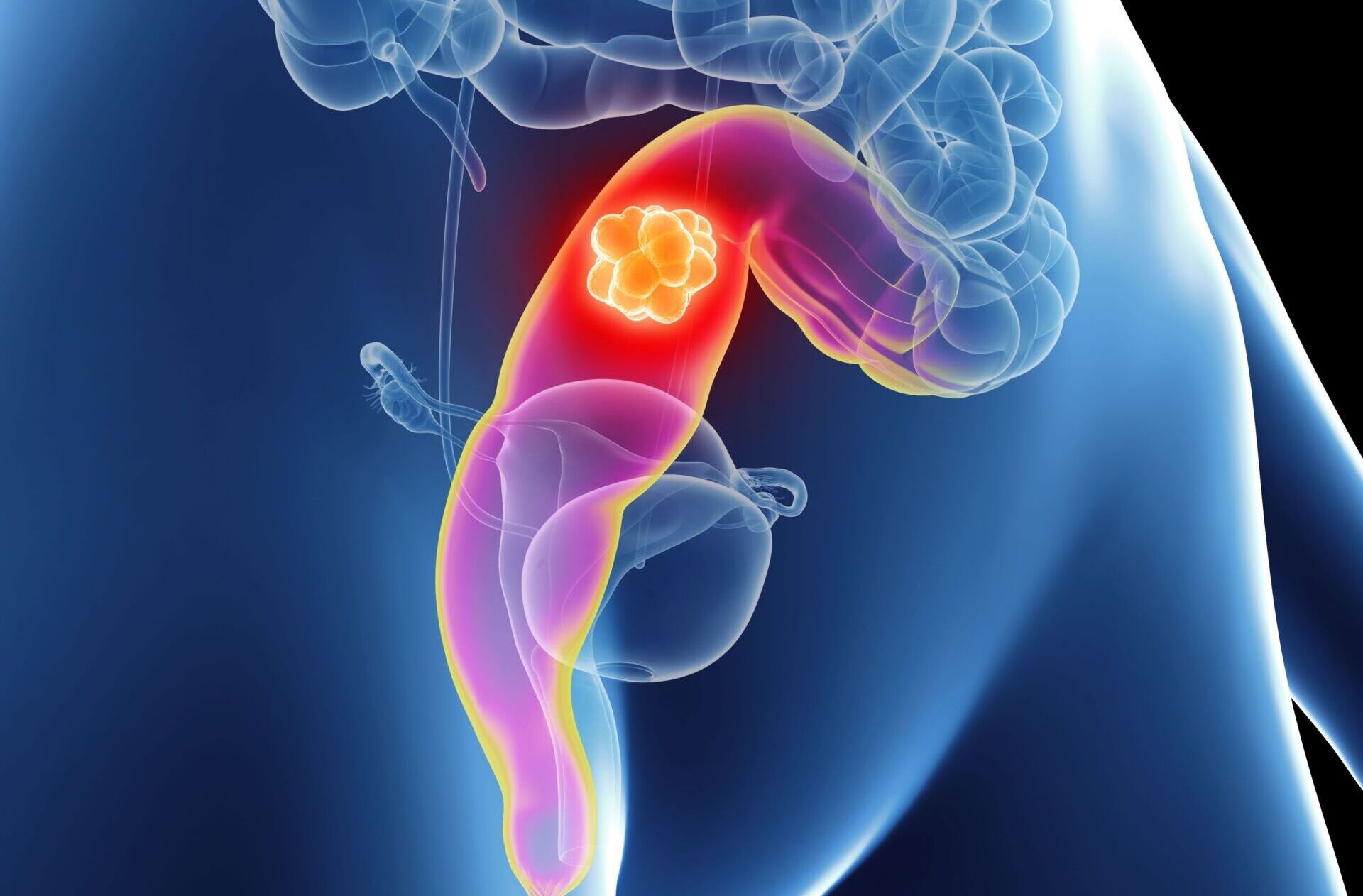
The intestine is just as important for the immune defense as for digestion. In the three to four meter long small intestine, digestive juices “break down” the food. Proteins, fats and carbohydrates as well as minerals and vitamins are absorbed here. This is done with the help of digestive juices. The large intestine extracts the water from the food pulp and thickens what is left. It also harbors trillions of bacteria that produce useful substances. Anatomically, the large intestine consists of several parts:
- Cecum: a short piece of intestine that lies in the lower right side of the abdomen and ends blindly. The “appendix vermiformis”, a small appendage, originates there.
- Large intestine (colon), consisting of ascending colon, transverse colon, descending colon and sigmoid
- Rectum
How common is colorectal cancer?
In Switzerland, more than 4,000 people are diagnosed with colorectal cancer every year. In this country, almost five out of every 100 women will be affected in the course of their lives, and about six out of every 100 men. Colon cancer is thus one of the most common tumor diseases in both sexes. Almost always it is colon or rectal cancer (colorectal cancer), small bowel cancer is rare. In around one in five people affected, the tumor has already formed visible offshoots at the time of diagnosis (stage
IV). Colorectal cancer is more common on the left side of the bowel than on the right. The following is important for diagnosis and treatment: Most intestinal tumors, namely around 60 to 70 percent, are located in the last thirty centimeters of this organ: in the descending part of the colon, in the sigmoid or in the rectum. Colorectal cancer almost always develops from (still benign) precancerous lesions that one day degenerate. These precursors are referred to as “polyps”, while the majority of them are adenomas, benign glandular growths. About one in five adenomas develops further in the course and can become dangerous. If adenomas are detected and removed in time, e.g. during a screening colonoscopy, up to 80 percent of colorectal carcinomas can be prevented. If colorectal cancer is diagnosed, the type of therapy and also the chance of cure depend on many factors. The tumor stage is important, indicating how deeply the tumor has penetrated the intestinal wall, whether lymph nodes are affected and whether metastases are present. Each affected person is therefore examined closely and in detail. Only a minority of colorectal tumors are detected at stage I, as symptoms almost never occur here. Most are not diagnosed until stage II or III. Then the cancer has already invaded all the walls of the intestine (stage II) or spread to adjacent lymph nodes (stage III). Colorectal cancer can metastasize via the bloodstream, especially to the liver and lungs. Through the lymphatic vessels, the cancer cells primarily reach nearby lymph nodes and, by direct spread, the peritoneum. However, when viewed under the microscope, these metastases are similar in nature to the so-called primary tumor in the intestine from which they originally originated.
Colorectal Tumor Center
At the USZ, numerous departments have joined forces to form a colorectal tumor center. The center is certified according to the guidelines of the German Cancer Society (DKG). A team of experts specializing in the medical care of colorectal cancer works closely together here for the benefit of our patients. At DKG-certified centers, patients are treated according to strict quality criteria and, according to current studies, have a better chance of survival on average.
What are the risk factors?
Age, genes, environmental factors, intestinal polyps and chronic intestinal inflammation – these five risk factors can promote colorectal cancer to a greater or lesser extent. The risk factor that usually weighs the most is age. From the age of about 50, the risk of disease increases steeply until the age of about 80. However, colorectal cancer is also becoming more common in young people (<40-50 years), suspicious symptoms must be consistently clarified even in young adults. One should be alert if adenomas appear before the age of 50. This is because the risk of colorectal cancer is then significantly higher not only for the affected person himself, but also for his parents and siblings. Adenomas that appear after the age of 60, on the other hand, are usually of no concern to relatives. Even if other cancers accumulate in the family, for example stomach cancer or uterine cancer, it makes sense to bring this up with the doctor. The likelihood of colorectal cancer increases more when several factors coincide. A healthy lifestyle can again reduce the risk. According to current knowledge, these influenceable factors include
- little movement
- daily consumption of red meat (raw, dried, processed into sausage or fried)
- moderate to high alcohol consumption (two or more alcoholic drinks per day or more than about 60 grams of alcohol per week).
- Smoking
- Overweight, especially a lot of belly fat
- Low intake of dietary fiber (e.g., from cereals, legumes, fruits, and vegetables).
The best recipe against bowel cancer is: sufficient exercise (preferably 30 to 60 minutes a day), a reasonable body weight, a healthy diet with sufficient fiber (preferably at least 30 grams a day), little alcohol and no smoking. This lifestyle statistically prevents about seven out of ten cases of colorectal cancer in men and four out of ten in women.
How does colorectal cancer show?
The insidious thing about colorectal cancer is that these tumors usually grow “silently” for a long time, so those affected do not notice anything. When colorectal cancer becomes apparent, the tumor has often grown unnoticed for years. That’s why early detection screenings are so important. Bowel cancer can manifest itself with these symptoms:
- Changes in bowel habits:
- Blood or mucus in or on the stool
- Diarrhea alternating with constipation
- newly appeared constipation
- Urge to defecate but no evacuation
- pencil thin stool
- tar black colored stool
- Anemia. The signs of anemia are fatigue, performance slump, skin pallor
- Recurrent abdominal pain and digestive problems
- Nausea, lack of appetite, feeling of fullness
- Weight loss even though you are not dieting
- Fever without signs of cold
Of course, everyone has digestive problems at some point. But if they persist or recur, they should be taken seriously. See your doctor if you notice warning signs of colorectal cancer and don’t put off this consultation – it can be lifesaving. Take a look in the toilet after every bowel movement. This way you will notice any bleeding sooner. Even though colorectal cancer is usually not noticeable for a long time. Nevertheless, both the precursors of the disease and colorectal cancer can be found with almost 100 percent certainty – provided that you look for them. This is what happens during “early detection.” Colorectal cancer screening is recommended in Switzerland for all individuals between 50 and 69 years of age. Risk groups (familial burden, chronic inflammatory bowel diseases) must be examined much earlier.
Second opinion colorectal cancer
When a cancer diagnosis is made, a second medical opinion is an important decision-making tool. The Comprehensive Cancer Center Zurich supports you with a professional expert opinion. They receive a thorough analysis of the situation as well as personal advice and quick answers to their questions.
What is the use of early detection?
Of the colorectal tumors detected during a screening examination, many are still at an early stage and are readily treatable. Then the chance for a cure is high. Two methods of screening are recommended for early detection in Switzerland: The blood-in-stool test and colonoscopy. These early detection methods provide the greatest benefit and are scientifically well tested. In the view of many experts, there are very good arguments in favor of colonoscopy. Although the stool test for hidden blood is less burdensome, it is not very sensitive, especially in early stages and pre-stages, Colonoscopy is the method with the best overall track record. Any colon polyps can almost always be removed immediately during colonoscopy. In terms of cost, both screening methods are comparable over the years. However, even the best early detection measure is of no use if it is not used regularly. Whichever one you choose: Get them done at the recommended intervals: Every two years for the fecal blood test and every ten years for the colonoscopy. If polyps have been found or if risk factors are present, the gastrointestinal specialist (gastroenterology) recommends closer monitoring.
How is colorectal cancer treated?
The treatment options for colorectal cancer are classically divided into three pillars:
- Surgery
- Radiotherapy
- Drug therapy/system therapy
To increase the effectiveness, several treatments are combined depending on the type, stage and spread of the intestinal tumor. The age and general condition of the affected person also play a role in the choice of therapies. The USZ specializes in state-of-the-art endoscopy and endoscopic tumor ablation, robotic minimally invasive surgery, innovative precision radiation, molecular oncology, immunotherapy and clinical trials. We offer forward-looking, multidisciplinary therapy concepts for the treatment of colorectal cancer according to the highest medical standards. We incorporate the latest scientific findings. An experienced team of experts from numerous disciplines is available to patients for consultation and treatment.
What are the chances of colorectal cancer?
Since about 1990, the prognosis in colorectal cancer has steadily improved and this trend is currently continuing. In stage I, the disease can be cured in more than nine out of ten people affected. Survival rates for advanced colorectal cancer have also improved in recent decades. Better and more early detection examinations have contributed to this, as have improved diagnostic methods, new surgical techniques, medications and other, new treatment methods. Switzerland is one of the countries with the highest survival rates for colorectal cancer.