Overview: What are cardiac arrhythmias?
There are several forms of cardiac arrhythmias:
- Tachycardic cardiac arrhythmia: The heart beats faster than 100 times per minute. The so-called tachycardic cardiac arrhythmias include atrial fibrillation, atrial flutter and ventricular tachycardia.
- Bradycardic arrhythmia: The heart beats less than 60 times per minute. This bradycardic arrhythmia, in which the heart beats too slowly, can occur, for example, if the heart is not supplied with blood properly or, in the aging process, the normal stimulus-generating or stimulus-conducting system is infused with nonfunctional connective tissue.
- Irregular heartbeat / skips: If the heart is out of rhythm and sometimes or constantly beats irregularly, the person concerned is suffering from a so-called arrhythmia. A common form of arrhythmia is extrasystoles – additional heartbeats that occur outside the regular rhythm. These extra beats are often harmless, but can be perceived as heart stumbling or an irregular pulse.
- Asystole: Pauses in the heart’s natural rhythm generator, the sinus node, lasting longer than three seconds.
We find out what type of cardiac arrhythmia is present based on a thorough examination.
What to do in the event of cardiac arrhythmia?
Whether a cardiac arrhythmia is harmless or dangerous can only be determined by a medical examination. Register now for an initial consultation and second opinion.
Symptoms: Palpitations and dropouts
This is how cardiac arrhythmias develop
The so-called sinus node is considered a natural pacemaker. It sets in motion the electrical excitations that make the heart beat. From the sinus node, impulses spread through the atria and throughout the heart. Damage to the sinus node has far-reaching consequences, as it can throw the heart’s regular beats out of sync.
In the same way, a disturbance in the so-called conduction system can lead to cardiac arrhythmias. This system is responsible for transmitting impulses from the sinus node to the heart muscle cells.
Cardiac arrhythmias: Causes and risk factors
The heart performs a very important task: it ensures the supply of oxygen to all organs and cells by pumping several thousand liters of blood through the circulatory system every day. Normally, it beats about 60 to 100 times per minute. If the affected person is currently under physical or psychological stress, there may be more beats. The human heart beats about three billion times in a long lifetime.
However, there are variations: In endurance athletes who train regularly, the pulse is generally lower at rest. Your heart is so powerful that fewer beats are sufficient to pump enough blood through your body. Here, even with significantly less than 60 beats, there are usually no pathological changes.
Heart disease and other diseases
Often, pronounced cardiac arrhythmias are based on a disease. Possible underlying heart disease:
There are many other diseases that at first seem to have nothing to do with the heart, but can affect it. These include:
Lifestyle and medication
Lifestyle can also affect the heartbeat. Those who drink too much coffee or alcohol, or are under constant stress, can develop cardiac arrhythmias. Some underlying organic diseases may exacerbate heart problems due to the additional stress. Also, medications you are taking for another condition may cause arrhythmias as a side effect. Therefore, we will ask you during diagnostics if you are currently taking any medications. In addition, drug use can also cause threatening cardiac arrhythmias.
Symptoms of cardiac arrhythmia
Cardiac arrhythmias have many faces. Some affected people hardly notice them and therefore do not worry. This is especially true if the heart beats slower or faster than usual only once in a while and the changes are minimal. A heartbeat that is very irregular, on the other hand, can already be perceived as threatening.
Typical signs of a cardiac arrhythmia are:
- Palpitations
- Heart stumble
- Dizziness
- Feeling faint
In addition to irregular heartbeats, other symptoms may occur. The symptoms that develop in individual cases depend on the type of cardiac arrhythmia.
Bradycardic arrhythmia – slow cardiac arrhythmia
If the heart beats too slowly, the body is no longer supplied with sufficient oxygen. This deficiency can manifest itself through various symptoms. For example through
- Decline in performance and weakness
- Vertigo: Affected individuals perceive illusory movements and sometimes have to sit down to avoid losing their balance. If this main feature is absent and the sufferers instead go black before their eyes, so that they have the feeling that they are about to fall and faint, this is known as presyncope.
- Circulatory collapse: The affected person becomes unconscious and faints. In this case, the rescue service should be called. The latter shall endeavor to ensure that no permanent damage is caused. Shortly before a fainting spell, you may experience signs such as dizziness, tunnel vision, tingling, heat, blurred vision and heart palpitations.
- Circulatory arrest: If the patient loses consciousness and no longer has a pulse or is no longer breathing, the emergency medical services should be called and resuscitation measures should be started immediately.
Tachycardic arrhythmia – rapid cardiac arrhythmia.
If the heart beats too fast, this leads to similar symptoms as if the heart beat is too slow. One may also feel weak and dizzy, and unconsciousness may also occur. In addition, some sufferers also experience increased nervousness. The heart beats strongly or even races.
Anyone who has symptoms of this type more often should see us. Even if the symptoms persist for a longer period of time, we need to clarify the causes behind the cardiac arrhythmia. Sometimes they are harmless, but they can also be signs of diseases that need treatment.
Diagnosis cardiac arrhythmia
First, we will ask you about symptoms and previous illnesses (medical history). After that, we will examine you to check if you have a cardiac arrhythmia. This also involves identifying the cause and possible consequences. We can use the following examination methods:
- Physical examination: we take your pulse and listen to your heart to detect any irregularities.
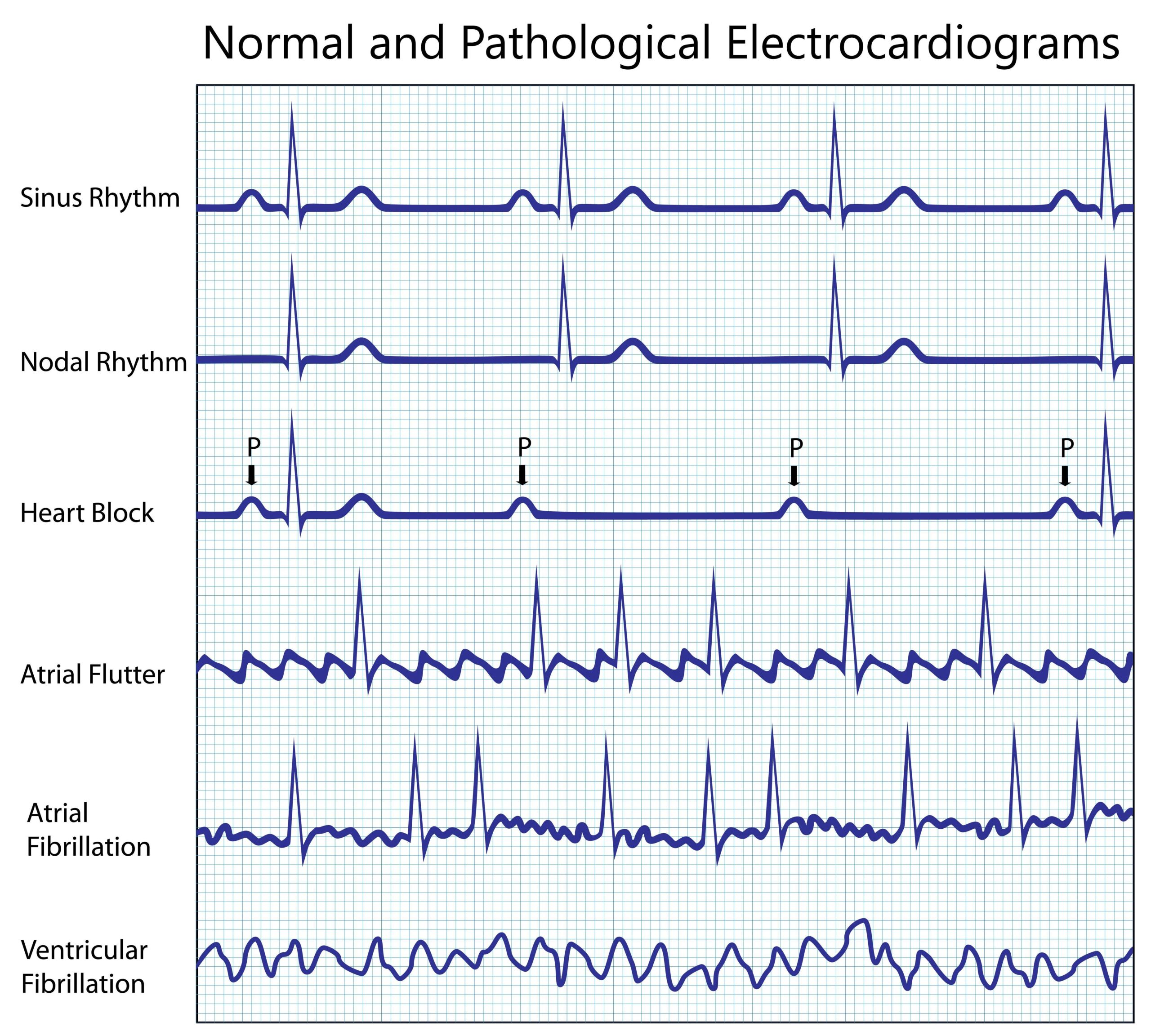
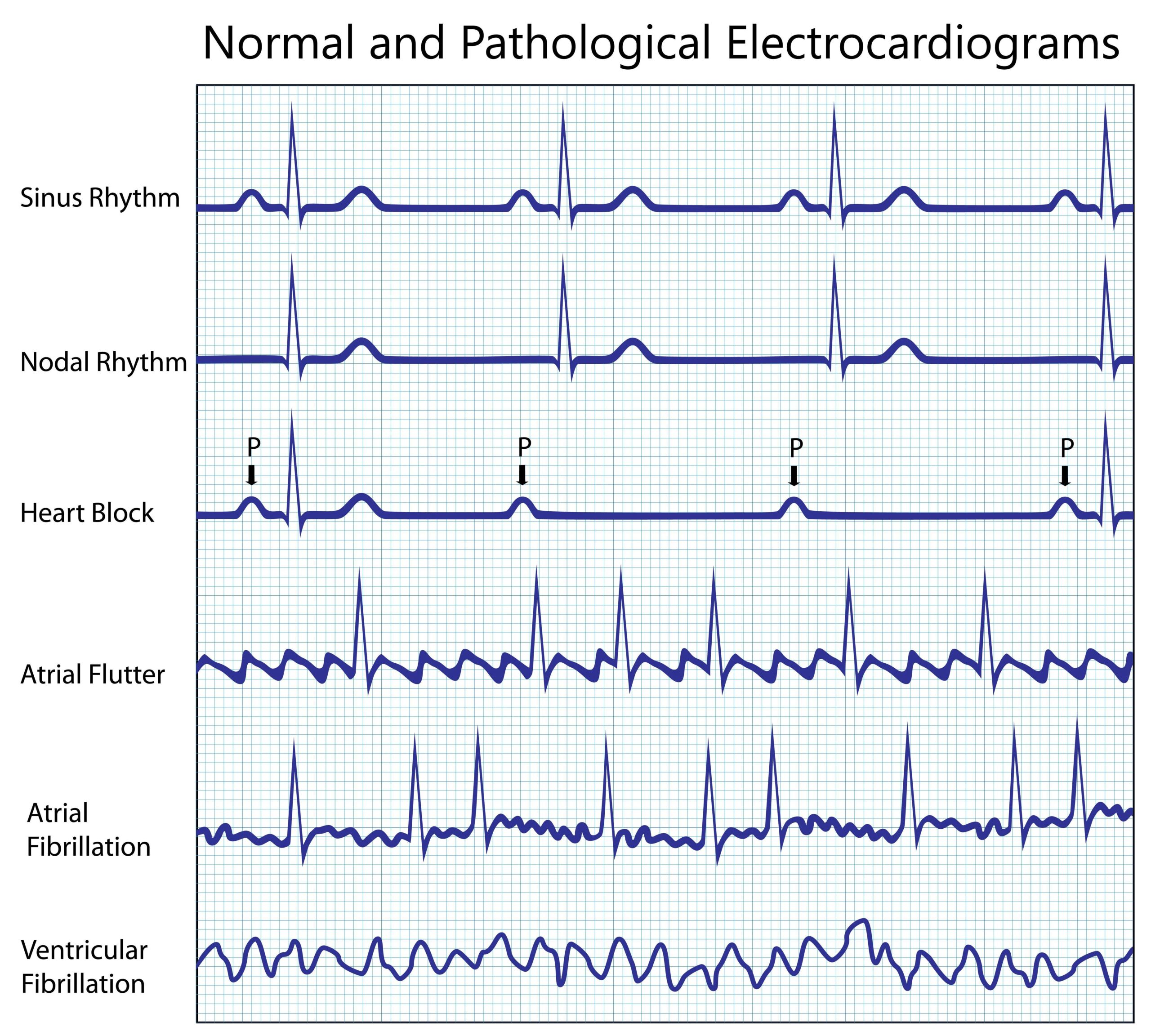
- ECG: The electrocardiogram provides accurate data about your heart function. Therefore, it is the most important examination when cardiac arrhythmias are suspected. We often order a long-term ECG to obtain data during the course of the day. To do this, you carry a small device with you for one to two days that measures the heart current curve and provides a pictorial representation.
- Exercise ECG= ergometry: During a step-by-step exercise protocol on a bicycle or treadmill, an ECG is derived and blood pressure is measured.
- Echocardiography: Using a heart ultrasound, we can check the structure and function of the heart. This is a routine examination that is neither painful nor dangerous.
- Electrophysiological examination of the heart (EPS): We measure the electrical impulses directly in the heart using a catheter.
- Blood tests
Initial consultation & second opinion Cardiac arrhythmia
Cardiac arrhythmias: Prevention, early detection, prognosis
With a healthy lifestyle, you reduce the likelihood of developing a cardiac arrhythmia. At the same time, you can reduce the risk of many other diseases and also improve your general health.
How to prevent cardiac arrhythmias
Here’s what you can do yourself for your heart health:
- Healthy diet: eat five hands full of fruits and vegetables every day. Also make sure to drink enough. Sweets, fatty foods and meat should only be put on the table in moderation.
- Sports: Exercise regularly. Go for a walk and keep fit with a sport. Having a hard time maintaining a regular workout? Try different sports so that you find one that you enjoy. At least half an hour a day should be devoted to sports.
- Avoid constant stress: Constant stress has a negative effect on your health. Make sure you balance your workout on a regular basis. Try methods that help you relax, such as autogenic training, progressive muscle relaxation or meditation. And make sure you have enough time for your family and hobbies.
Course and prognosis (cardiac arrhythmias)
Cardiac arrhythmias can progress differently depending on the type and cause. In many cases they are harmless and do not impair the heart’s pumping capacity. They often cause no or only mild symptoms, such as an occasional heart stumble, and therefore usually pose no direct risk to health.
However, there are also more serious forms of cardiac arrhythmia that prevent the heart from pumping enough blood through the body. These can lead to dizziness, fainting, shortness of breath or, in extreme cases, life-threatening complications such as heart failure or sudden cardiac death. Arrhythmias that occur in the heart chambers (ventricles) are often more serious than those that occur in the atria.
The prognosis depends largely on the underlying cause and the general state of health of the person concerned. With timely diagnosis and appropriate treatment, many cardiac arrhythmias can be well controlled or even remedied. Individual therapy tailored to the cause is important in order to prevent complications and improve quality of life. In severe cases, devices such as pacemakers or defibrillators may be necessary to minimize the risk of serious events.
Treatment for cardiac arrhythmias
Even people with a healthy heart repeatedly notice that their heart beats unusually. This is not a cause for concern and does not require treatment.
Therapy is useful if certain diseases underlie the cardiac arrhythmia. If, for example, the symptoms are due to advanced heart failure, there is a risk of sudden cardiac death. In this case, immediate treatment is required. The same applies if the symptoms of the cardiac arrhythmia are so severe that they affect your everyday life and dizziness attacks occur again and again or the heart beats felt up to the neck.
Details of the treatments
FAQ on the topic of cardiac arrhythmias
Some arrhythmias in patients without underlying heart disease can be stopped in acute cases using breathing techniques such as vagus stimulation (e.g. deep breathing and gentle pressing, increasing abdominal pressure). In severe cases in patients with serious structural heart disease, emergency medical treatment, such as medication or electrical cardioversion, is necessary.
If your pulse is irregular, you should sit down and relax. If the irregular pulse lasts longer or is accompanied by symptoms such as dizziness, shortness of breath or chest pain, medical advice should be sought immediately.
Cardiac arrhythmia can manifest itself in heart stumbling, palpitations, irregular pulse, dizziness, fainting, shortness of breath or chest pain.
Heavy physical exertion and excessive stress should be avoided, especially without medical clarification. The consumption of caffeine and alcohol can also aggravate cardiac arrhythmia.
Cardiac arrhythmias can be caused by electrolyte disturbances, such as a lack of potassium or magnesium. These minerals are important for the electrical activity of the heart.
Stress, lack of sleep, alcohol, caffeine and certain medications or drugs can aggravate cardiac arrhythmias. Untreated underlying illnesses such as high blood pressure or thyroid problems can also worsen the situation.
The treatment depends on the cause. Lifestyle changes, such as stress management, a healthy diet and avoiding triggering factors, sometimes help. In more severe cases, medication, catheter ablation or implantable devices such as pacemakers may be necessary.