What is autoimmune thyroiditis or Hashimoto's thyroiditis?
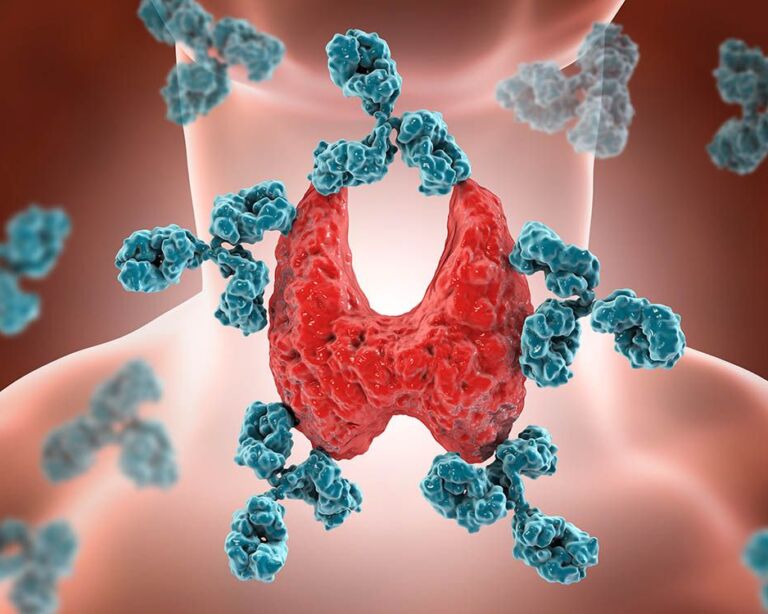
This is an inflammatory reaction of the thyroid gland. The body’s own defense system mistakenly targets thyroid cells. The immune system therefore attacks the body’s own tissue. This persistent autoimmune reaction leads to the destruction of thyroid tissue over a period of years. The chronic inflammation therefore reduces the size of the thyroid gland over time, the organ works less and less and hypothyroidism develops.
This can have a whole range of negative consequences for the entire metabolism. Incidentally, the most common cause of hypothyroidism is autoimmune thyroiditis or Hashimoto’s thyroiditis.
Autoimmune thyroiditis – frequency and age
Chronic thyroiditis often only occurs in adulthood, usually from the age of 30 and up to 50. Women are often affected; their risk of developing this form of thyroiditis is around 5:1 compared to men.
The terms autoimmune thyroiditis stand for autoimmune thyroid inflammation and Hashimoto’s thyroiditis is named after the Japanese physician Hakaru Hashimoto, who was the first to describe this thyroid disorder as an independent disease around 100 years ago. Colloquially, the disease is often abbreviated to “Hashimoto’s”.
Autoimmune thyroiditis: causes and risk factors
Autoimmune thyroiditis or Hashimoto’s thyroiditis refers to an autoimmune disease that is directed against the thyroid gland.
Defense cells such as T lymphocytes attack the thyroid gland as if it did not belong to the body but to foreign tissue. Due to the involvement of T lymphocytes, this autoimmune disease is also known as chronic lymphocytic thyroiditis.
The triggers that misdirect our immune system and cause it to produce antibodies against thyroid tissue are still unknown. But there are assumptions:
- Familial predisposition: Genes could play a role, as autoimmune thyroiditis or Hashimoto’s thyroiditis occurs more frequently in some families. Some of those affected also have other autoimmune diseases, which confirms the theory of a family history. These include type 1 diabetes and celiac disease, but also rarer autoimmune diseases such as Addison’s disease (adrenal hypofunction), vitamin B12 deficiency anemia or pernicious anemia, but white spot disease (vitiligo) can also be present in parallel with autoimmune thyroiditis or Hashimoto’s thyroiditis. If at least two organs that are part of the hormone balance or two different glands are restricted in their function or no longer work, we speak of a polyglandular autoimmune syndrome, for example in type 1 diabetes and thyroiditis. The term polyglandular is made up of the Greek words “poly” for many and “glandula” for gland.
- Iodine-rich diet: If there is a family history of thyroid disease, a diet particularly rich in iodine could also be a risk factor for the development of thyroid autoimmune disease – contrary to popular belief that a diet rich in iodine is good for the thyroid gland.
- Infections: An infection with certain bacteria or viruses could trigger the familial predisposition to develop an autoimmune thyroid disease, so to speak.
A genetic predisposition plus an infection could therefore be the cause of this autoimmune thyroid disease, it is assumed, but this has not been proven.
Initially sometimes like hyperthyroidism, later typical of hypothyroidism
Autoimmune thyroiditis or Hashimoto’s thyroiditis often remains undetected for a long time because there are virtually no early symptoms. The chronic disease progresses slowly. Mild hyperthyroidism can sometimes occur in the early stages as a response to the inflammation. The following symptoms then appear, which are typical of hyperthyroidism:
- You sweat more than before.
- Although you are not eating less than usual, you are losing weight.
- You are nervous.
- You are constantly suffering from palpitations.
As autoimmune thyroiditis progresses, thyroid tissue is destroyed and the production of thyroid hormones decreases. This results in the specific symptoms of an underactive thyroid (hypothyroidism), such as
- The drive is missing.
- You gain weight and tend to become constipated.
- This leads to concentration problems.
- You are constantly tired, even though you sleep more than before.
- They shiver quickly and are particularly sensitive to the cold.
- The skin becomes dry.
- The hair also changes and becomes brittle.
Autoimmune thyroiditis or Hashimoto’s thyroiditis alter the thyroid gland. This can cause the organ to shrink (atrophy of the thyroid gland), but sometimes it can also enlarge. The enlargement of the thyroid gland is often perceived by those affected as an additional symptom, as a so-called globus sensation in the throat. They describe it as if a lump is pressing in the throat and narrowing the pharynx a little.
Autoimmune thyroiditis: diagnosis at the USZ
Because the symptoms only become clearer gradually, most sufferers do not seek medical advice until it is too late. Thyroid inflammation is therefore often only diagnosed when the organ is already noticeably damaged and its function is restricted.
Three main methods are used to detect thyroid inflammation such as autoimmune thyroiditis or Hashimoto’s thyroiditis:
- Palpation examination: During the palpation examination, we check whether the thyroid gland is enlarged or reduced in size and whether it is sensitive to pressure. Palpation can therefore already provide initial clues.
- Blood test: The blood test is more informative if autoimmune thyroiditis or Hashimoto’s thyroiditis is suspected. These include various blood values that are associated with the thyroid gland. On the one hand, this involves a targeted search for specific antibodies that occur in autoimmune thyroiditis. They indicate whether this disease is present, but not whether thyroid function is also affected. This is why thyroid levels are also checked, as they show whether and to what extent the chronic inflammation is already affecting thyroid function. Together, these values provide information on whether Hashimoto’s thyroiditis is present and to what extent it results in a thyroid dysfunction that requires treatment. A typical example of the detection of autoimmune thyroiditis and the associated hypothyroidism: TSH and TPO-AK values are elevated, T4 values are too low.
- Ultrasound examination: Finally, the ultrasound examination provides additional information on whether the thyroid gland is altered by inflammation. In addition, further examinations can be carried out, such as fine needle biopsy for tissue sampling and thyroid scintigraphy as an imaging diagnostic option.
- Scintigraphy: A thyroid scintigraphy can also be used to obtain information about the function of the thyroid gland.
Autoimmune thyroiditis: prevention, early detection, prognosis
Targeted prevention of Hashimoto’s thyroiditis is not possible. Because the causes of this chronic thyroid disease are not known, there are no reasonable starting points in this context.
Therefore, do not fail to recognize the disease at least as early as possible. Always have the symptoms listed checked by a doctor. The simple blood test checks the most important thyroid parameters safely and quickly.
Course and prognosis of autoimmune thyroiditis
There is no way to cure Hashimoto’s thyroiditis. The chronic inflammation progresses and gradually destroys thyroid tissue. This results in hypothyroidism. However, this can be compensated for with appropriate tablets.
Autoimmune thyroiditis only becomes dangerous if this therapy is not carried out. However, if the thyroid dysfunction is treated and specifically compensated for, those affected can live normally and are considered healthy.
Self-help groups
The exchange with people who are affected by the same disease can be a great support in coping with the disease. Advice on finding a suitable self-help group is available from Selbsthilfe Zürich. Self-Help Zurich and the University Hospital Zurich are cooperation partners in the national project “Health literacy thanks to self-help-friendly hospitals”.
Hashimoto's thyroiditis: treatment with thyroid hormones
Autoimmune thyroiditis does not always need to be treated. Because even if the antibody values are high – as long as the thyroid values are normal, i.e. the thyroid gland is functioning well, no medication is necessary. However, if elevated antibody levels have already been detected, you should have your thyroid levels checked annually to be on the safe side, so that any dysfunction can be detected early and countermeasures can be taken.
The special thing about this chronic thyroid disease is that it is not the disease itself that is the target of the therapy; the inflammation cannot and does not need to be treated, but its symptoms, caused by the hypothyroidism as a result of the inflammation.
Only when hypothyroidism occurs is treatment necessary, namely in the form of hormone replacement therapy, which can compensate for the lack of thyroid hormones. L-thyroxine (levothyroxine) is used as the active ingredient, with the dose depending exactly on how severe the deficiency of this hormone is.
You should have your thyroid levels checked at regular intervals to ensure that the amount is optimal. In most cases, thyroid function continues to decline over the course of a person’s life, which is why the dose of the hormone medication needs to be adjusted. Of course, the medication usually has to be taken for the rest of the patient’s life because thyroid tissue that has already gone under does not recover, so the hypothyroidism remains and has to be compensated for.