What are anal fistulas?
Anal fistulas are unnatural ducts that form between the anal canal and the skin around the anal opening. As a rule, the ducts form due to inflammation of special glands in the anal canal, the proctodeal glands. In humans today, they are only incompletely and individually laid out in varying numbers. They may even be missing altogether. However, there are other causes of anal fistulas, for example chronic inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis.
A fistula in the anal area can be very unpleasant: Affected persons usually feel pain and secretions flow out of the opening of the fistula. In addition, the area around the fistula may become red and swollen due to the inflammation.
Anal fistulas often form as a result of anal abscess, due to purulent inflammation caused by bacteria. Anal fistulas and anal abscesses are essentially the same condition. Anal abscess is accompanied by an encapsulated collection of pus and corresponds to the acute form. Anal fistula, on the other hand, is the chronic variety in which the purulent fluid leaks out through an opening in the skin.
Anal fistulas usually do not heal on their own. Treatment usually consists of surgery, for which there are various techniques. Which of these doctors choose depends on the type and course of the fistula. Without surgical treatment, there is a risk that the fistula will become inflamed and pus will form. And the well-being and quality of life of those affected also suffer.
Anal fistulas – frequency and age
Anal fistulas are relatively common. Experts estimate that around 20 out of every 100,000 inhabitants contract the disease every year. The frequency appears to vary within Europe, as a study from 2007 showed: the population in Spain developed anal fistulas the least frequently (1.04 per 10,000 inhabitants/year). The highest rate was in Italy (2.32 per 10,000 inhabitants/year).
Affected by the unnatural ducts in the anal region around the sphincter are mainly adults between 30 and 50 years. Men are affected significantly more often due to the increased number of proctodeal glands.
Anal fistulas: Causes and risk factors
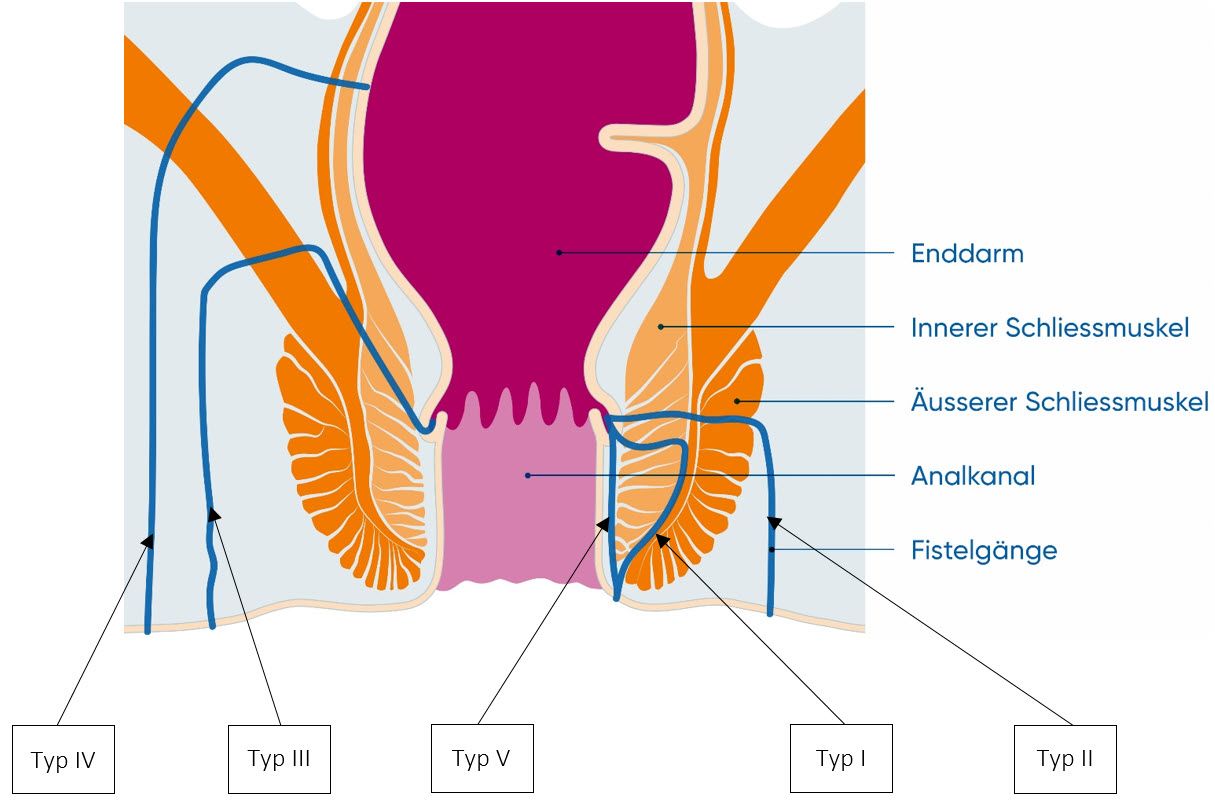
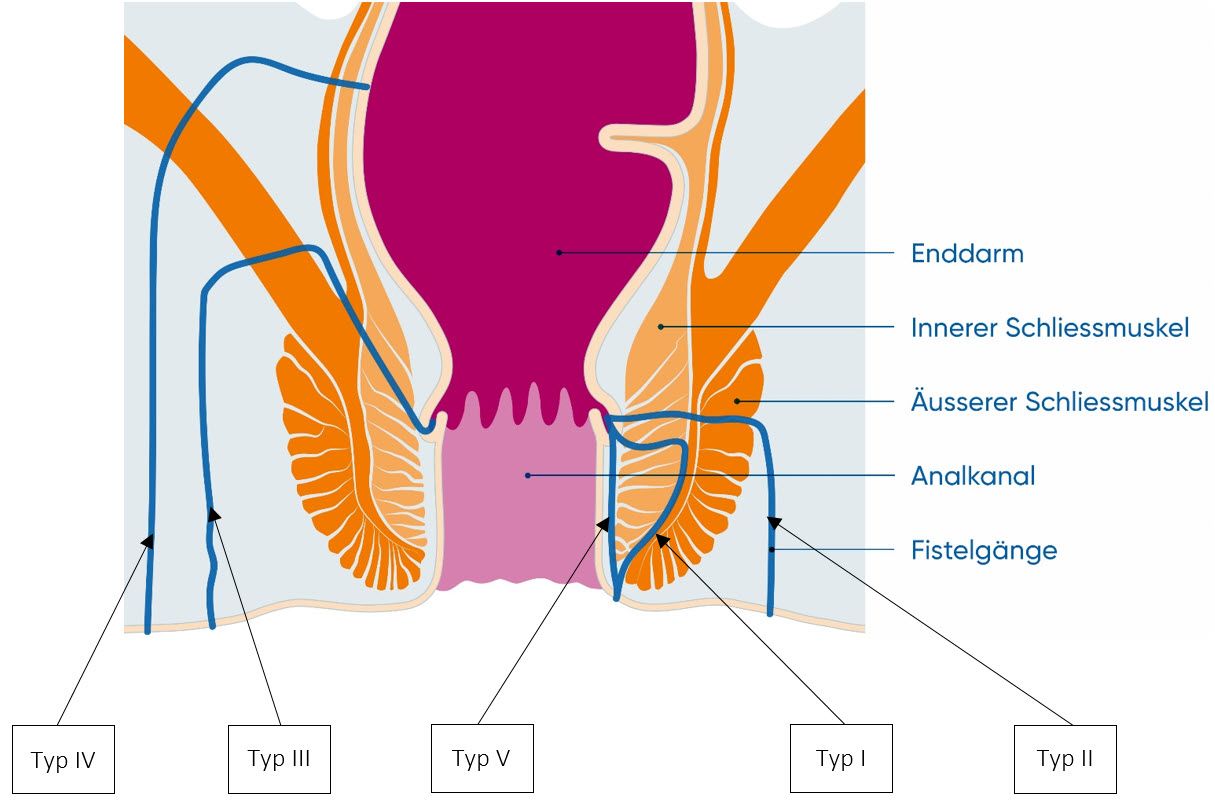
The most common cause of anal fistulas is infection of the proctodeal glands with bacteria. The inflamed glands eventually become a long duct and fistula. Anal fistulas can take very different routes to the skin surface and progress in different ways. According to the Parks classification, anal fistulas are divided into five different types – depending on their course in their relationship to the sphincter muscle (Musculus sphincter ani):
- Intersphincteric anal fistulas (type I) are very common. The ducts run between the internal and external sphincter.
- Transsphincteric anal fistulas (type II) are common. The ducts completely penetrate both sphincters, i.e. both the internal and external parts.
- Suprasphincteric anal fistulas (type III) are rare. The ducts run between the sphincter and pelvic floor muscles.
- Extrashphincteric anal fistulas (type IV) are very rare. The fistula ducts do not involve the sphincter muscle and originate outside the anal canal.
- Submucosal (subanodermal) anal fistulas (type V) run directly under the mucosa and do not involve the sphincter.
Risk factors for anal fistula
According to recent findings, there are some risk factors that are believed to promote anal fistulas. These include, for example:
- Obesity
- Diabetes
- Dyslipidemia
- Skin diseases
- high consumption of very spicy food
- high daily salt consumption
- Smoking
- Alcohol consumption
- lack of exercise, sitting for long periods of time
- prolonged sitting on the toilet during defecation
- psychosocial stress
Anal fistula symptoms
Anal fistulas can cause some very unpleasant symptoms. The following complaints are possible:
- Pain, especially when sitting and having a bowel movement
- The fistula persistently leaks secretions that may contain pus. Patients may be disturbed by the odor and oozing that contaminates the underwear.
- Bleeding
- Itching
- Symptoms of inflammation: Fever as well as redness, overheating and swelling of the anal region.
- If the fistula is very large, wind or stool may escape.
Do not be afraid to see a doctor if you have such symptoms, because a fistula usually does not disappear by itself.
Anal fistulas: Diagnosis with us
The diagnosis of an anal fistula always begins with a discussion of the patient’s medical history, the anamnesis. The doctor will ask you some questions, such as:
- What are your symptoms? e.g. pain, secretion in the anal region
- When did the complaints first appear?
- How intensively are they pronounced?
- Do the complaints improve in between or do they persist continuously?
- Do you have any known diseases? e.g. inflammatory bowel disease, HIV, infections, cancer
- Lifestyle: How do you eat and how much do you exercise? Are you a smoker? How much alcohol do you drink?
- Previous surgeries: Have you ever had surgery in the anal region or have you had any diseases in this area? If so, which ones?
From your answers, doctors can usually already draw conclusions as to whether it could be an anal fistula.
State-of-the-art diagnostics and treatment
At the USZ, we offer the entire spectrum of treatment for proctological diseases. We work in an interdisciplinary manner with various clinics and centers and offer state-of-the-art diagnostics and treatment. We are one of two centers in Switzerland offering stem cell treatment for perianal fistulas caused by Crohn’s disease.
Anal fistulas: Prevention, early detection, prognosis
The cause of anal fistulas in most cases is inflammation of the proctodeal glands. And this one you can not prevent. You also have few options for prevention in the case of other diseases such as Crohn’s disease or cancer. You may be able to work on a healthy lifestyle, as some factors seem to promote anal fistulas. Some tips:
- Move as much as possible in everyday life and do sports.
- If your job requires you to spend a lot of time sitting – make sure you get enough exercise in between.
- Make sure you eat a healthy diet with plenty of fruits, vegetables and whole grains. Use less salt and be cautious with spicy foods.
- Give up smoking, and if you are a smoker: Try to stop smoking.
- Drink alcohol only in moderation and take regular alcohol breaks.
There are no known special measures for early detection of anal fistula. Always see your doctor if you notice pain or purulent secretions in the anal region. In this way, you prevent inflammation and purulent abscesses from repeatedly forming and the anal fistula from taking a chronic course.
Course and prognosis in anal fistula
Anal fistulas usually do not heal on their own. Surgery is usually required to achieve definitive closure of the fistula.
The consequences can be repeated inflammations and anal abscesses. Anal fistulas can also affect the rectum. In up to one third of cases, the sphincter muscle at the anus is damaged – there is a risk of more or less pronounced fecal incontinence. Even after surgery in which doctors split the fistula (fistulotomy), the risk of fecal incontinence may be increased if the sphincter was not working properly before. A rarity is the formation of a fistula cancer or a fistula carcinoma in very long existing fistulas.
Anal fistulas: Treatment by surgery
Treatment of anal fistula consists of surgery. Only very rarely does it heal again without therapy. There are several surgical techniques. The method surgeons use depends on the type of anal fistula, its course and especially in relation to the sphincter. The aim is always to preserve the function of the sphincter and to heal the anal fistula permanently.