Extensive tumor burdens traditionally considered inoperable are now amenable to curative treatment by systemic conversion chemotherapies, followed by a variety of interventions such as enlargement of the healthy liver by portal vein occlusion, staged surgery(ALPPS) or ablation modalities.
Liver transplantation is established in selected patients with hepatocellular carcinoma, but is also becoming a promising option for many other tumor types such as perihilar cholangiocarcinoma, neuroendocrine or colorectal liver metastases.
Future treatment will be based on personalized approaches based on molecular tumor subtyping, response to targeted drugs, novel biomarkers and precision surgery adapted to the specific tumor. (Reference: Modern therapeutic approaches for the treatment of malignant liver tumors. Nat Rev Gastroenterol Hepatol. 2020; 17: 755-772)
Swiss HPB Center
The treatment of liver cancer at the University Hospital Zurich (USZ) is carried out by highly qualified specialists in cooperation with all medical departments. These include liver surgery, hepatology and gastroenterology, oncology, radiotherapy and radiology. The USZ offers the latest and most effective treatment options for liver tumors and is also a certified liver cancer center. The treatment of all patients is embedded in the structures of the Liver Tumor Center at the Comprehensive Cancer Center Zurich (CCCZ) and the Swiss Center for Liver, Pancreatic and Biliary Tract Diseases (Swiss HPB Center). Patients with liver tumors are discussed with all medical disciplines at a tumor board specially designed for liver tumors. The optimal and individual treatment is determined for each patient.
Surgical therapy approaches
There are various surgical approaches to the treatment of liver cancer.
Liver resection
The treatment of liver cancer has benefited from a large number of innovations. However, liver surgery (liver resection) remains the best option for long-term survival and cure of various primary and secondary liver tumors, mostly hepatocellular carcinoma (HCC), intrahepatic cholangiocarcinoma (ICC) and perihilar cholangiocarcinoma (PHC) as well as colorectal liver metastases (CRLM). Success in complex cases depends on an optimal combination of different therapeutic approaches in the right order to either cure patients or enable long-term survival and a satisfactory quality of life.
In contrast to all other solid organs, the liver can rebuild a new, fully functional tissue mass (liver regeneration) within a short time after a major tissue loss, such as during an operation. This ability is the basis for the feasibility of large hepatectomies (liver resections), in which up to 80 % of the liver tissue is removed from patients with healthy livers. The main obstacles to early liver surgery were uncontrolled bleeding during resection and insufficient liver volume or insufficient liver function. The use of anesthesia with low central venous pressure, occlusion of the inflow (e.g. with the Pringle maneuver), improvements in surgical techniques and a precise knowledge of the segmental liver anatomy were central to the progress of modern liver surgery.
Parenchyma-sparing liver resection is based on the principle of preserving non-tumorous liver tissue, e.g. in tissue-preserving procedures such as portal vein embolization (PVE) or portal vein ligation (PVL). The basic idea behind this less invasive approach is the presumed higher tolerability of liver surgery and a lower risk of postoperative liver failure (hepatic insufficiency). A further advantage is the potentially greater feasibility of repeat liver surgery in the event of tumor recurrence.
Liver surgery strategies tailored to specific tumor scenarios: Most liver tumor removals can be achieved through a single surgical procedure, sometimes involving extensive resection preceded by percutaneous portal vein embolization (PVE). (Reference: Modern therapeutic approaches for the treatment of malignant liver tumors. Nat Rev Gastroenterol Hepatol. 2020; 17: 755-772):
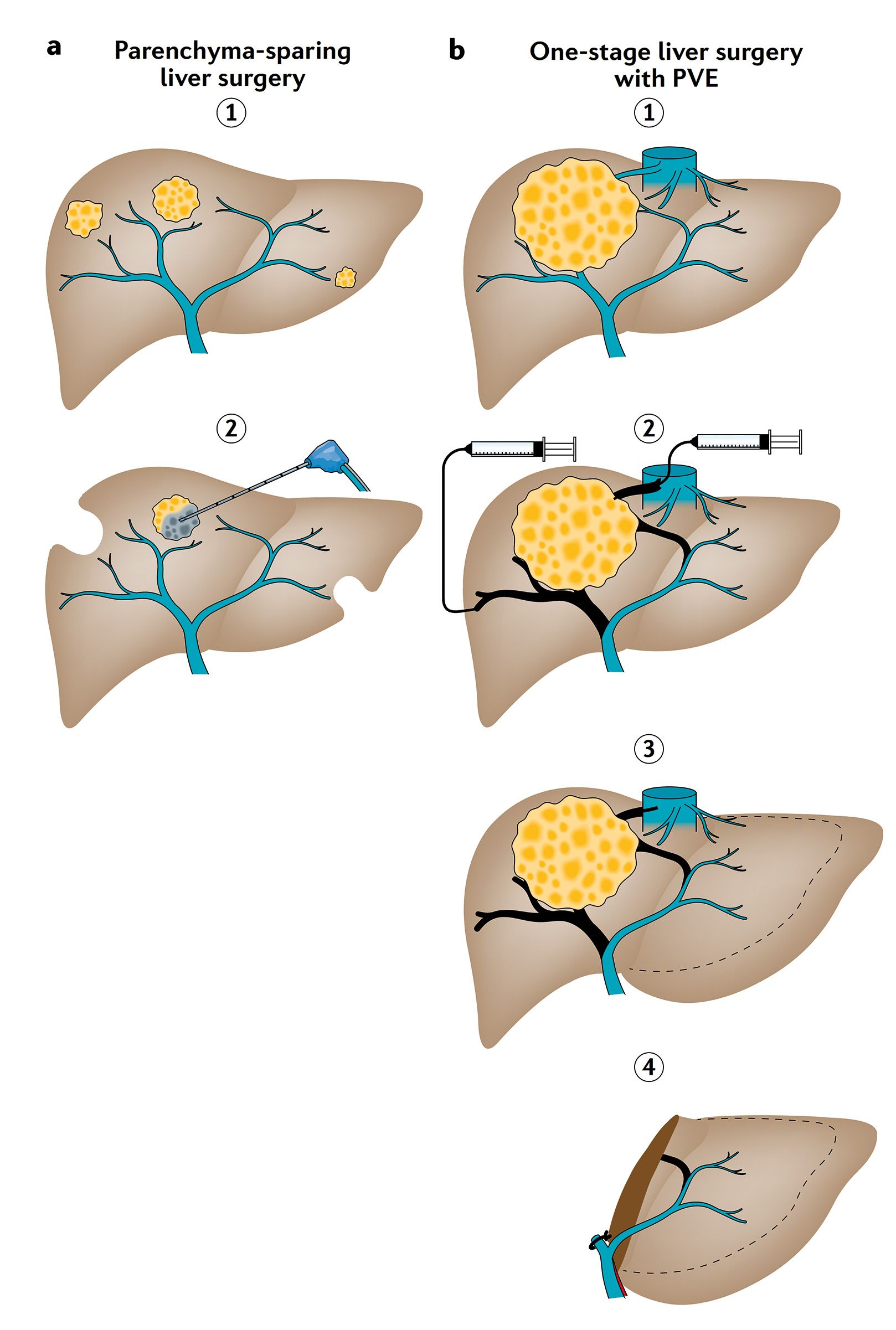
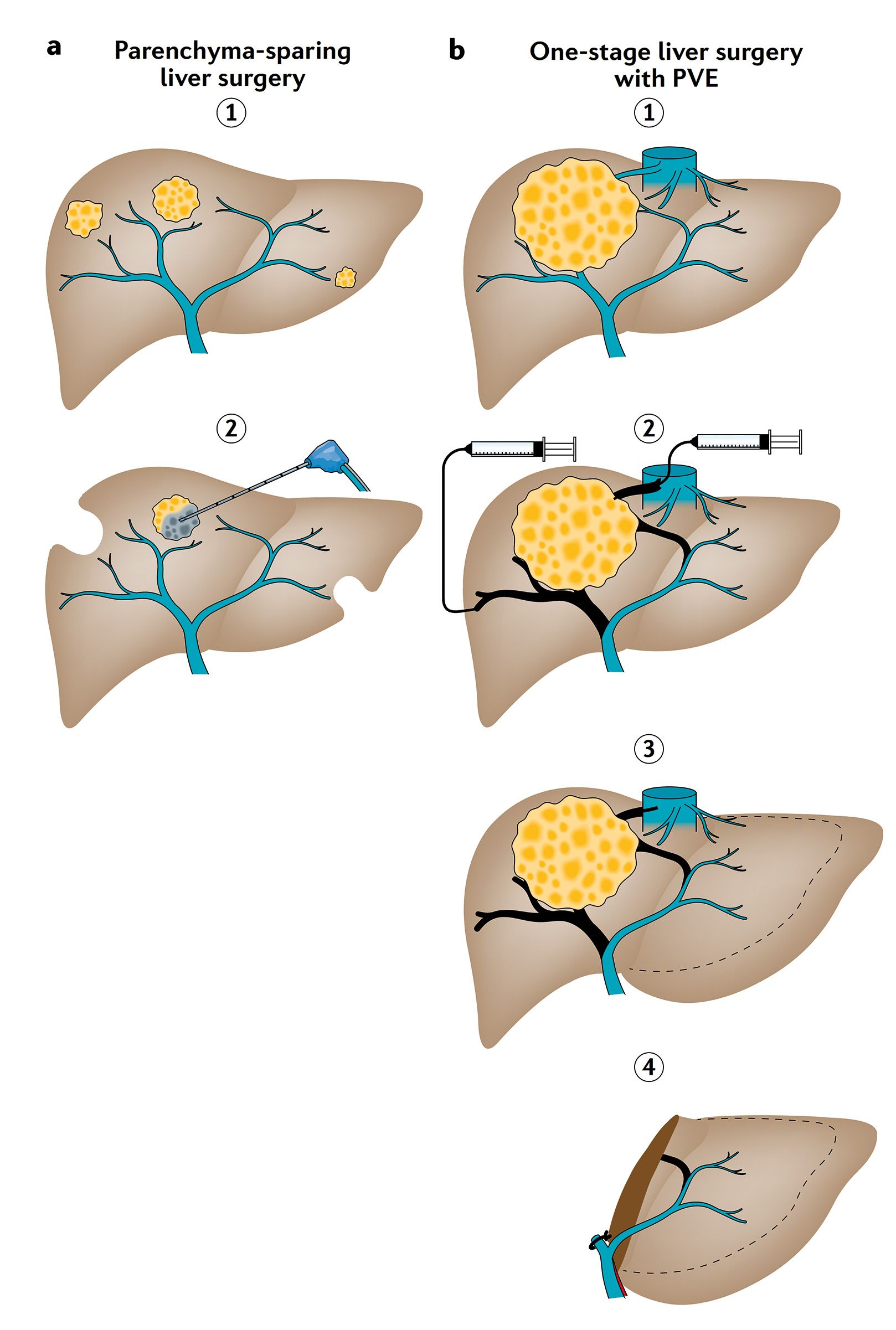
Figure A and B:
Limited hepatic tumor burden, with either unilobar (single tumor) or bilobar distribution (multiple tumors/metastases) (step 1), may be best removed individually with or without ablative tumor destruction (step 2). This single-stage resection is referred to as “parenchyma-sparing liver surgery” (part a). Tumours that are suitable for single-stage resection but have a small future liver remnant (FLR; e.g. < 25-30 %) (step 1) require tissue augmentation by portal vein embolization (PVE) and sometimes additional hepatic vein embolization of the tumour-bearing side of the liver (step 2). Once sufficient volume hypertrophy of the FLR has been achieved (step 3, part b), typically 4-8 weeks after PVE (with or without hepatic vein embolization), a complete hepatectomy can be performed (step 4, part b).
However, some patients, particularly those with multiple colorectal liver metastases (CRLM) in which both sides of the liver are affected, are not suitable for a single-stage surgical procedure (hepatectomy). This requires a two-stage surgical procedure (Reference: Modern therapeutic approaches for the treatment of malignant liver tumors. Nat Rev Gastroenterol Hepatol. 2020; 17: 755-772):
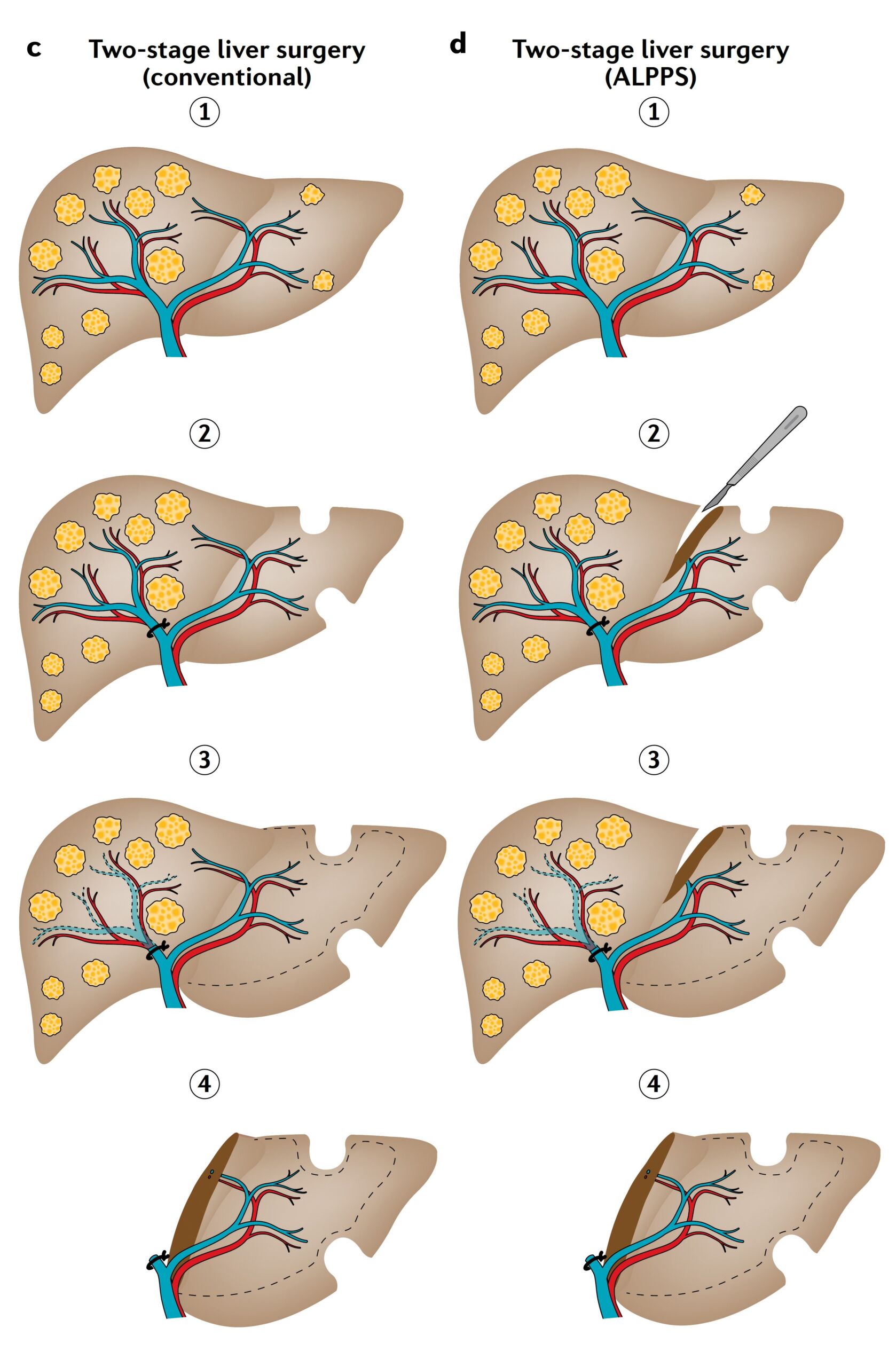
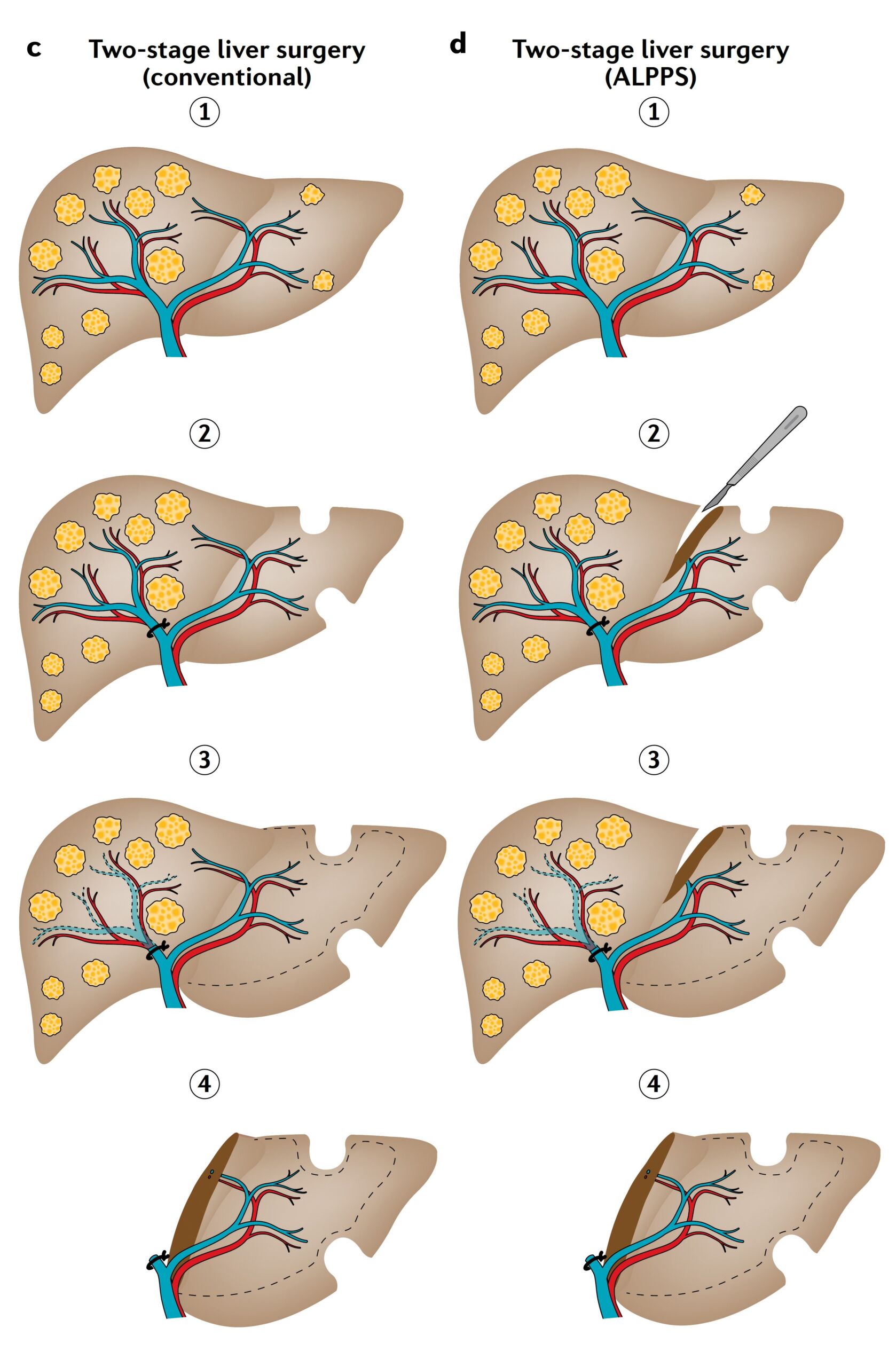
Figure C and D:
Extensive tumor burden affecting both sides of the liver (step 1) is often treated with two-stage hepatectomies (liver surgery) either by conventional hepatectomy (partial c) or by combining liver partition and portal vein ligation for staged hepatectomy (ALPPS) (part d). In both types of hepatectomy, tumor removal of the liver remnant (FLR) is combined with portal vein ligation in the first stage of the operation (part 2). In ALPPS, the operation is supplemented in the first stage by a liver transsection (part d, step 2). Once sufficient volume hypertrophy has been achieved (step 3) the complete hepatectomy is performed in the second phase (step 4) carried out. While the inter-stage interval for conventional hepatectomy is typically 4-8 weeks (part c, steps 2-4), ALPPS triggers rapid growth so that complete hepatectomy can be performed 7-14 days after the initial surgery (part d, steps 2-4). The size of the initial FLR (dashed line) is projected onto the enlarged FLR to illustrate the effect of volume hypertrophy (parts c-d, steps 3,4).
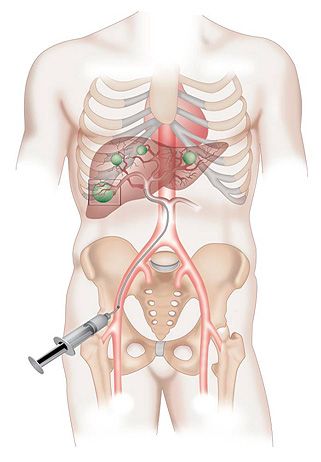
Portal vein embolization (PVE) to enlarge the residual liver
Computed tomography of the liver three months after intra-arterial chemotherapy and ligation of the right portal vein in a patient with hepatocellular carcinoma.
In critical cases, preoperative preparation (about 3 weeks before the operation) is sometimes necessary. If the residual volume after resection is too small, the remaining part of the liver is stimulated before the operation by closing the portal vein on the other side of the part of the liver to be removed by interventional radiologists (preoperative embolization). This leads to a redistribution of blood flow in favor of the remaining portion and thus enables compensatory growth (hypertrophy) before the operation.
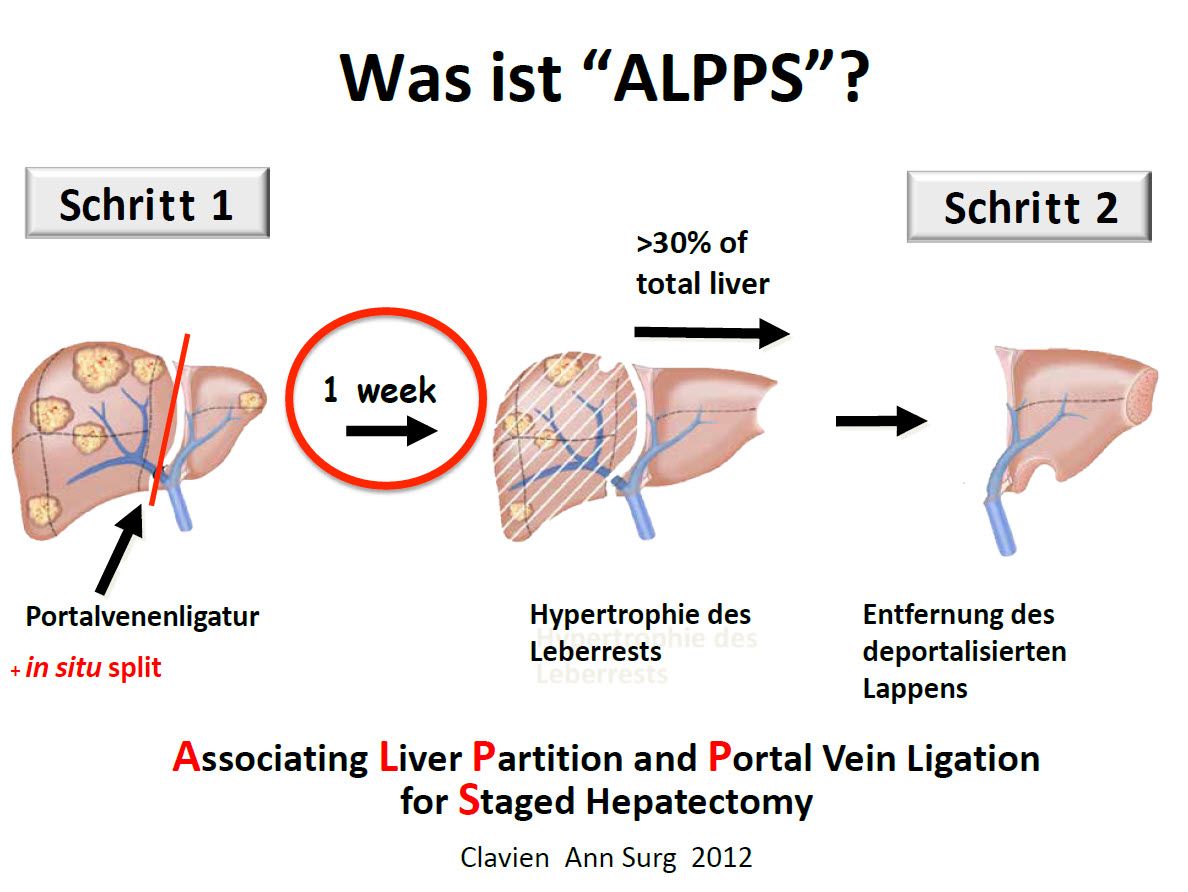
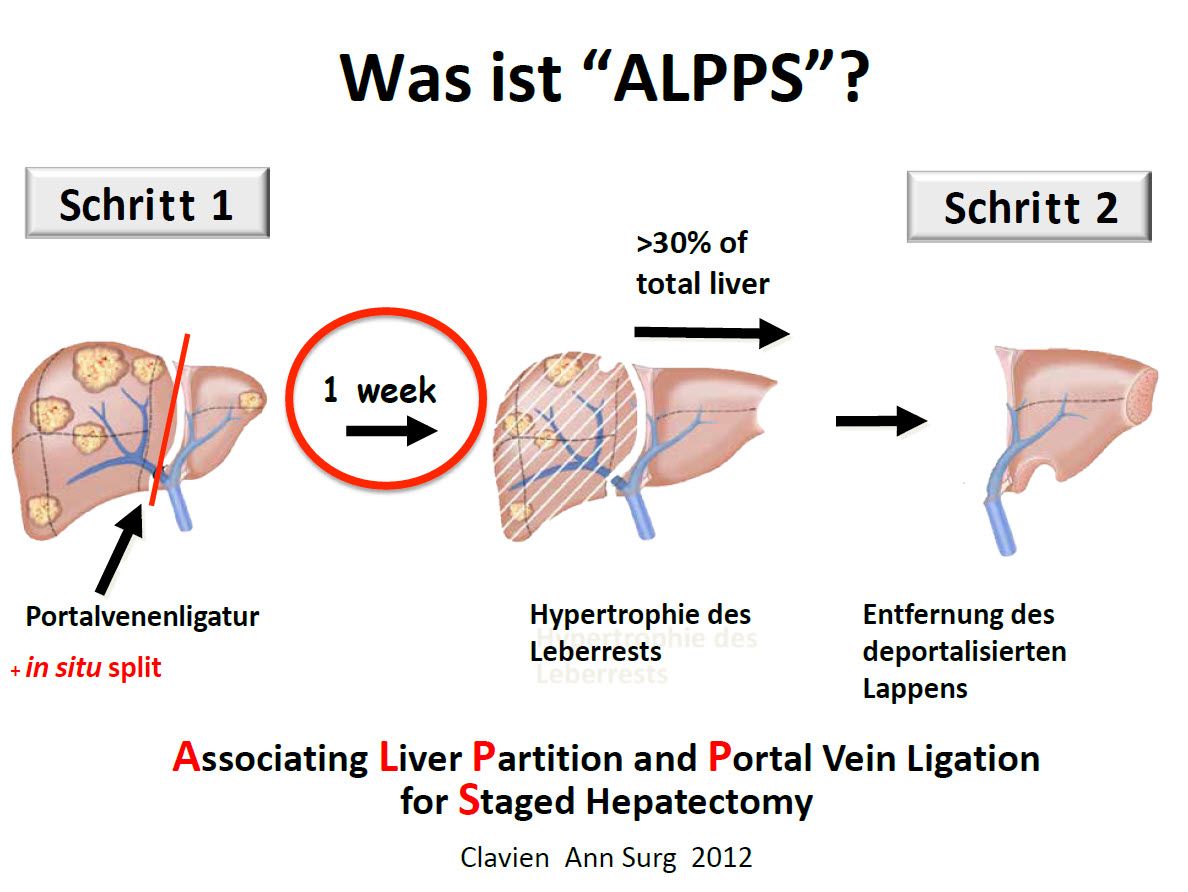
Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy (ALPPS) to enlarge the remaining liver – Promising results in the fight against liver cancer
Since 2011, we have also been performing a new method of liver resection in Zurich, which allows us to remove up to 80-90% of the total liver in two operations with a short time interval of 1-2 weeks between the operations in the case of very small residual liver volumes. The growth of the liver is stimulated by dividing the liver without resection in a way that can normally only be achieved after a complete liver resection, without the liver being completely resected. Only in the second step is the affected liver completely resected.
Detailed explanation of the ALPPS operation
Laparoscopic liver surgery
In liver surgery, too, many resections are now performed using minimally invasive methods, i.e. with only a few small incisions (so-called keyhole technique or laparoscopy). For this purpose, a camera is inserted into the abdomen and long instruments are used to operate on the parts of the liver that need to be removed. Ultrasonic dissectors are usually used to cut through the liver tissue. The pieces of liver are then removed from the abdomen through a small incision in the lower abdomen. The operation is usually shorter, blood loss is generally less and patients can often go home earlier. Laparoscopic liver resection has become a standard of care, with data suggesting equivalent oncologic outcomes and better postoperative recovery compared to open liver resection. However, laparoscopic liver resection also has limitations that must be taken into account when planning the operation.
Highest precision through robot-assisted liver surgery (da Vinci ®)
Another minimally invasive procedure is robot-assisted liver surgery (da Vinci). Like classic laparoscopy, it uses small access points through which the camera and instruments are inserted. With the da Vinci surgical system, the surgeon sits at a control console from which he or she receives a full HD 3D view via the video system and guides the four arms of the robot. The strengths of the da Vinci surgical system lie in the exact representation of the anatomical structures and the extreme mobility of the robotic instruments, which make it possible to remove liver tumors with high precision.
Robot-assisted surgery with the da Vinci surgical system (da Vinci XI) established itself in liver surgery in 2019. Since then, patients undergoing oncological liver surgery in particular have benefited from this state-of-the-art, minimally invasive procedure. The da Vinci surgical robot enables the surgeon to perform even very complex operations where classic laparoscopy reaches its limits, despite the smallest incisions.

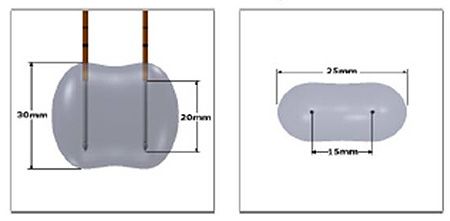
NanoKnife
The NanoKnife system uses irreversible electroporation (IRE). This is a new type of technology that involves a series of rapid electrical impulses. These impulses trigger the opening of the cell membranes in the cancer.
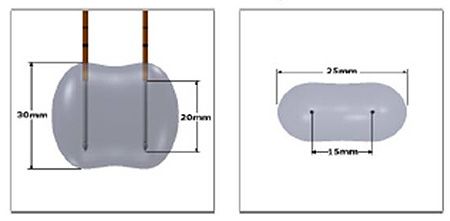
Application of NanoKnife technology: The electricity flows between the electrodes in a dumbbell-shaped field.
These pores are permanently disrupted by the high voltage and contribute to the cell death of the cancer cells. The great advantage of the NanoKnife system is the greatly improved protection of tissue, especially nerves, blood vessels and bile ducts, which was not possible with all previous ablation systems such as radiofrequency ablation (RFA) or microwave ablation. Ablation therapies are used in the treatment of both primary and metastatic liver tumors.
Detailed explanation of the NanoKnife
Liver transplantation for hepatocellular carcinoma (HCC)
Today, liver transplantation is one component of the highly developed multimodal therapy methods available to treat many patients with advanced primary or secondary liver cancer. Hepatocellular carcinoma is currently the only widely accepted cancer indication for liver transplantation. HCC is also the most common indication in many transplant programs and currently accounts for up to 40% of all patients waiting for a liver transplant in Europe. The main cause of HCC is liver cirrhosis of any etiology, which significantly impairs the function and regenerative capacity of the liver. Liver transplants can be performed either from cadaveric donors or living donors.
The gold standard in the treatment of HCC is surgical resection, but many patients are not eligible for this treatment due to the advanced stage of the disease. Transplantation can be an alternative to resection in patients with non-resectable tumors without liver cirrhosis; in patients with decompensated cirrhosis, transplantation is the best curative option. The treatment of patients in the compensated liver cirrhosis stage is the subject of controversial debate.
On the basis of an international consensus conference on HCC held in Zurich in 2010, we recommend liver transplantation as the treatment of choice for patients with liver cirrhosis, even if the tumor is resectable. Transplantation has advantages over liver resection in patients with HCC: a cirrhotic liver is replaced by a normal liver, the development of new tumorous parts within the cirrhosis is prevented and portal hypertension is cured.
Nevertheless, liver transplants are not available to all patients due to the limited number of donors. In recent years, there has been growing interest in live liver transplantation for hepatocellular carcinoma in order to reduce mortality on the waiting list. The advantages of living liver transplantation are a better overall condition of the recipient, better graft function and shorter waiting times. At the University Hospital Zurich, living liver transplantation is offered to patients with small HCC and liver cirrhosis, thereby reducing mortality and improving long-term survival.
We also perform liver transplants on patients with perihilar cholangiocarcinoma, the so-called “Klatskin tumor”, and have achieved good results with this procedure. We strictly adhere to the strict selection criteria developed at the American MAYO CLINIC for the transplantation of these tumors, some of which are very difficult to remove by resection (“Mayo criteria”).
Radiofrequency therapy, chemoembolization, SIRT
Locoregional treatments destroy the tumor cells locally in the liver without the need for surgery: They can sometimes be used together with resections to avoid having to remove so much tumor tissue. This procedure can be performed percutaneously (through the skin) or during surgery and is suitable for tumors less than 5 cm in size.

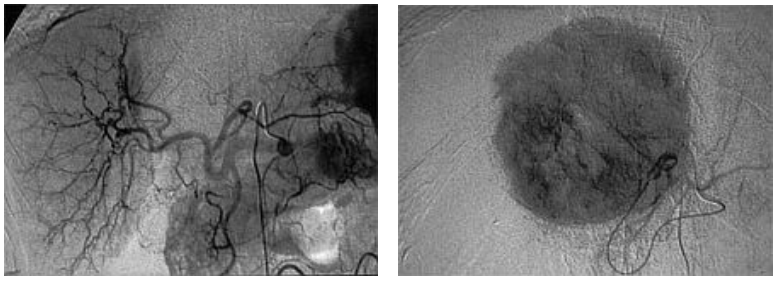
Ultrasound-guided radiofrequency ablation of a liver tumor
Radiofrequency therapy
Radio waves are used to generate heat within the tumor, causing the cells to burn.
Percutaneous ethanol injection
Alcohol is injected directly into the tumor to destroy it.
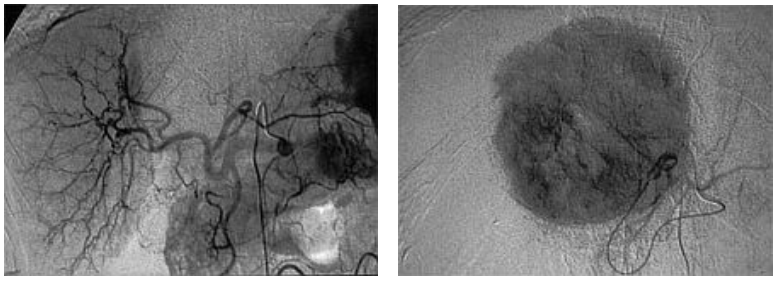
Chemoembolization
Chemoembolization is an interventional procedure performed by radiologists. A branch of the hepatic artery is closed off by small plastic particles. The blood supply is reduced and the tumor is no longer supplied with sufficient oxygen. In addition, the tumor can be treated with local chemotherapy, which can significantly reduce the systemic effects of conventional chemotherapy.
This therapy option is suitable for patients on the waiting list for a liver transplant, before a liver resection or for non-operable patients.
Radioembolization
SIRT stands for “Selective Internal Radio Therapy” and is an innovative form of treatment for malignant liver tumors.
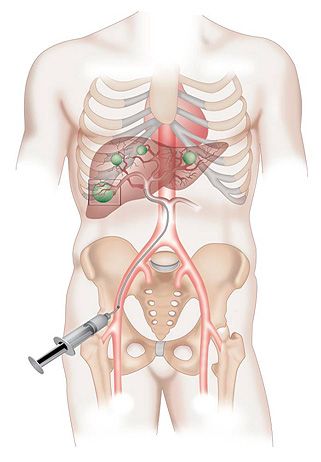
The treatment is a promising option for patients whose liver tumors cannot be treated with local procedures (such as surgery) and no longer respond adequately to chemotherapy. Here, the nuclear medicine team at the USZ and the interventional radiologists inject small radioactive plastic beads (loaded with yttrium-90) directly into the arteries that supply the tumor. Over the next 72 hours, these beads begin to kill the tumor.
In SIRT therapy, microspheres loaded with yttrium-90 are introduced into the hepatic artery via the large body arteries and applied directly to the tumor, where they emit gamma rays over the next 72 hours.
Aftercare
After resection or local treatment of a hepatocellular carcinoma, a check-up using computer tomography or magnetic resonance imaging and a blood test (AFP) every 3-6 months is recommended in order to detect a recurrence (reappearance of a tumor) at an early stage.