Definition of chronic constipation
At least 2 symptoms during at least 12 weeks of the previous 6 months, in a quarter of bowel movements:
- Lumpy or hard stools
- Feeling of incomplete bowel evacuation
- Feeling of anal blockage
- Manual maneuvers to facilitate defecation (evacuation with the finger, support of the pelvic floor)
- Less than 3 bowel movements per week
- Soft stools only with laxatives
- Insufficient criteria for irritable bowel syndrome
What are the causes of constipation?
The causes of constipation seem to be clear. Too little fluid intake, too little fiber in the diet and too little exercise were previously blamed as the main factors that can lead to constipation. This could also explain why constipation occurs mainly in the older population. Unfortunately, however, these explanations seem to be based on myths that are passed on from one generation to the next. To date, there are no good scientific studies to support these hypotheses. The cause of constipation appears to be much more complex than previously thought.
In principle, constipation can be divided into primary and secondary constipation.
Primary constipation
- normal transit time
- Delayed transit time
- Outlet-Obstruction
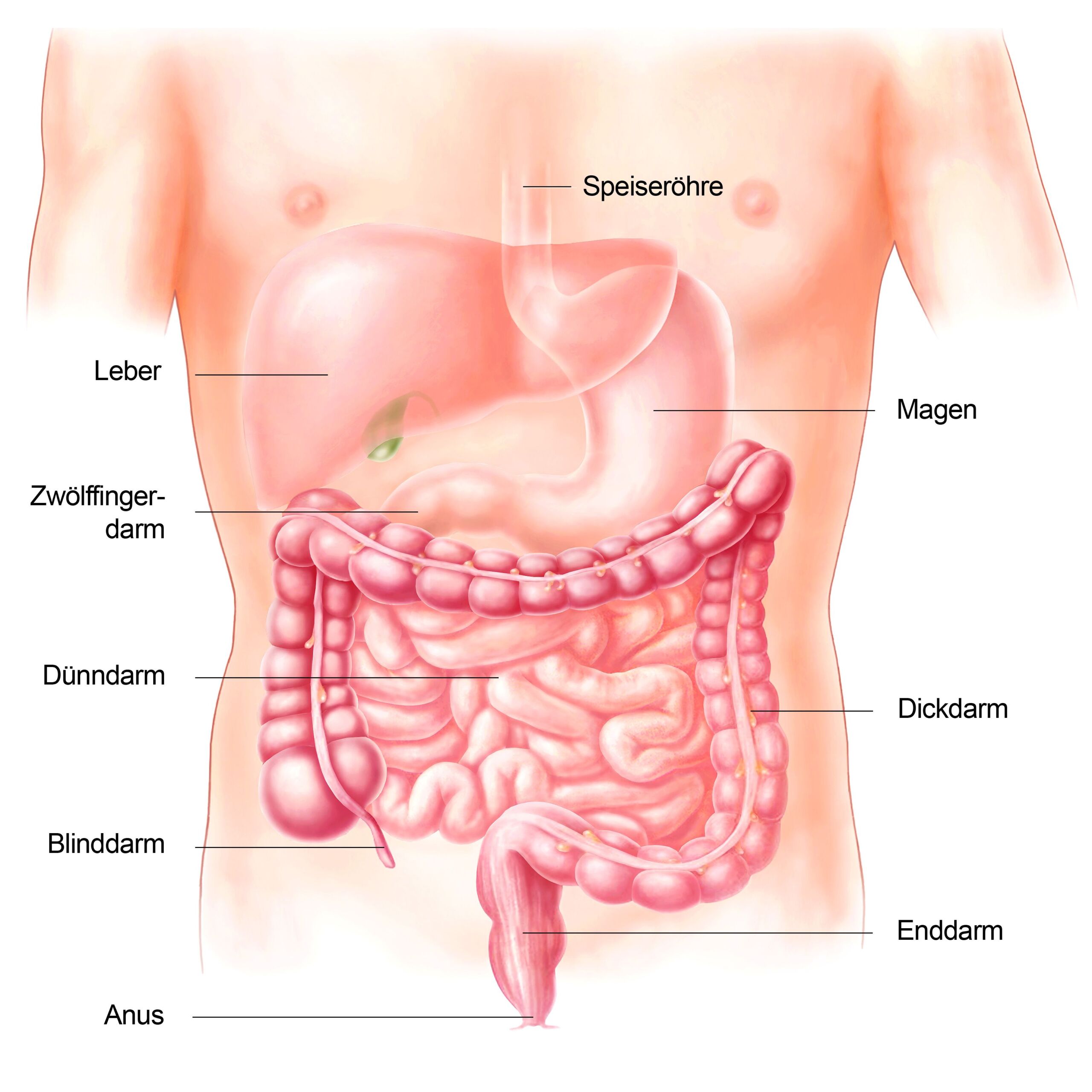
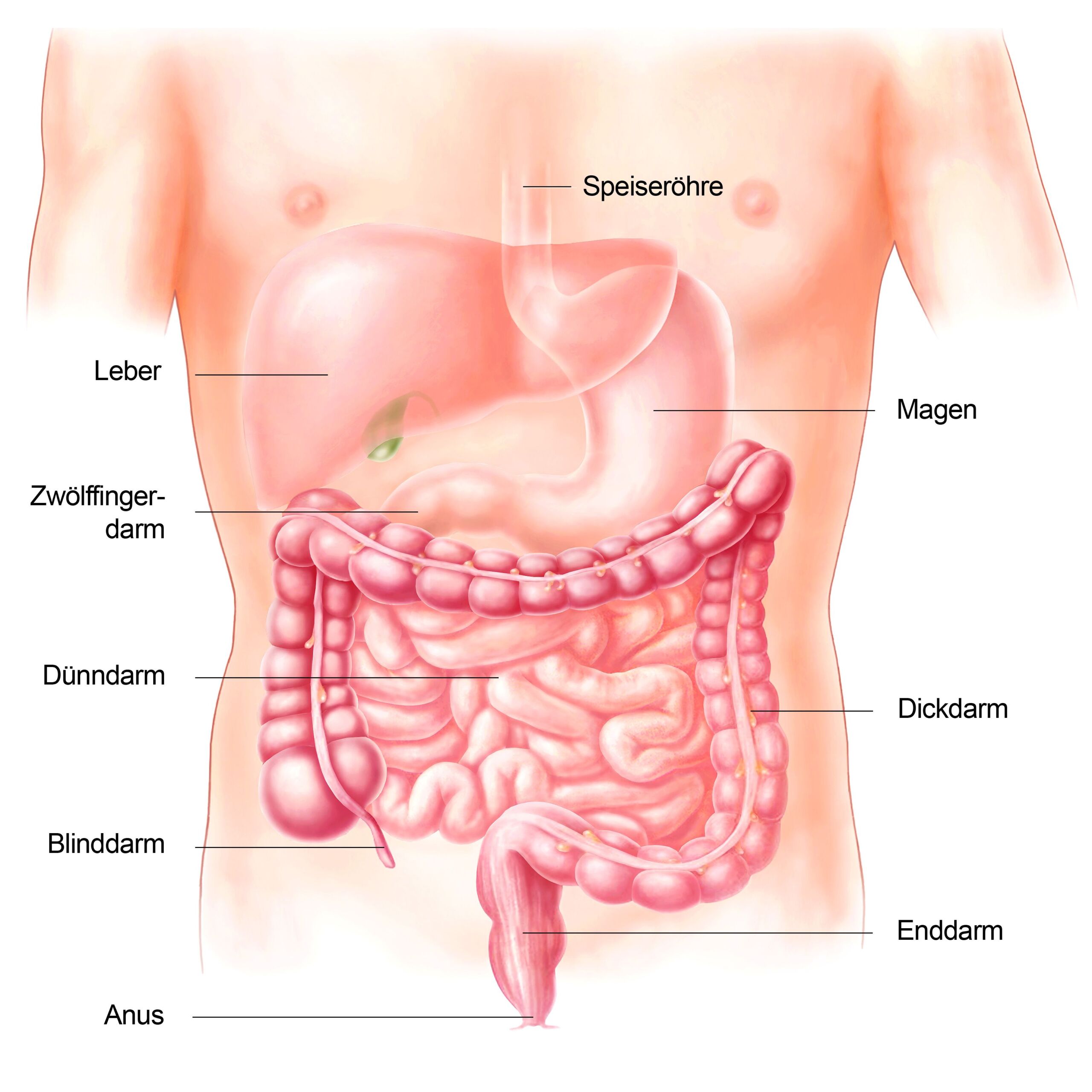
The primary causes can be divided into 3 groups: Constipation with normal transit time (also called functional constipation), constipation with delayed transit time (“sluggish bowel” or “slow transit constipation”) and constipation due to a pelvic floor disorder (so-called “outlet obstruction”). Functional constipation is the most common type, in which the time of intestinal passage for the stool is normal. As a rule, this passage time is less than 72 hours. In constipation with delayed transit time, the predominant symptom is infrequent bowel movements, often combined with flatulence. Disorders of the nerves that regulate the bowel are discussed as the cause. Constipation due to a pelvic floor disorder is caused by dysregulation of the pelvic floor muscles, which makes it difficult to evacuate the stool. This type of constipation is characterized by a feeling of blockage or incomplete bowel evacuation. Sometimes patients can only pass stool with manual assistance by inserting a finger into the anus or vagina to push the stool out of the rectum.
Secondary constipation
Hormonal disorders/metabolic diseases
Anatomical change
Neurological diseases
- Multiple sclerosis
- Parkinson’s
- M. Hirschsprung (nerve disease of the intestine)
Psychiatric disorder
Drug-related
- Opiates (morphine or morphine-like)
Secondary constipation is less common than primary constipation. The direct causes of constipation are other diseases such as diabetes mellitus, thyroid and parathyroid disorders, psychiatric disorders (depression), irritable bowel syndrome or bowel cancer. The last two secondary disorders are of particular importance. Irritable bowel syndrome is very common and mainly affects young women. Irritable bowel syndrome is a dysregulation of the entire gastrointestinal tract, often accompanied by cramps but also episodes of diarrhea. The cause is unknown and treatment is difficult.
Colon cancer is an important diagnosis to rule out in the investigation of constipation. In a study in which over 500 patients with constipation were examined, colorectal cancer was found in 1.4 % of patients, and possible precursors of this, so-called adenomas, in 20 %.
When and how should constipation be clarified?
If a patient meets the criteria for chronic constipation, secondary constipation should be ruled out first. The extent of the assessment depends on the exact symptoms, the patient’s age and any accompanying symptoms. The decisive factor is the questioning of the individual Rome III criteria, in particular the question about hard bowel movements, the feeling of incomplete bowel evacuation and the use of the fingers to evacuate the rectum. These symptoms or circumstances are often not spontaneously reported by the patient. In addition to a precise assessment of the symptoms, a finger examination of the rectum can be very informative. In addition to a possible tumor – around a third of all bowel cancers can be felt with the finger – a statement can be made about the function of the pelvic floor. All patients with chronic constipation should be questioned in detail and examined with a finger. Whether a blood sample should be taken to rule out hormonal disorders or a colonoscopy should be performed depends on the accompanying symptoms and age. From the age of 50, all patients with constipation should have a colonoscopy, unless they have already had a colonoscopy in the last 5 years. A colonoscopy can also be considered for patients between the ages of 40 and 50. A colonoscopy is only necessary for patients under the age of 40 if family members have a history of colorectal cancer.
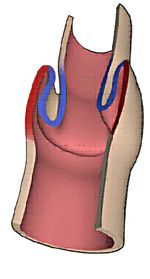 Examination of the pelvic floor using magnetic resonance (so-called MR defecography) has become indispensable in the diagnosis of chronic constipation. With MR defecography, the movements of the pelvic floor and all its parts (bladder, vagina, uterus, rectum, small intestine) can be precisely tracked and displayed as a film sequence. This examination is particularly indicated for patients who are suspected of having a pelvic floor disorder or an “outlet obstruction”. An “outlet obstruction” is a constipation where the cause lies at the end of the bowel, at the exit of the bowel so to speak. Constipation is caused by a disorder of the pelvic floor if there is incorrect coordination of the pelvic floor muscles or an internal bowel prolapse.
Examination of the pelvic floor using magnetic resonance (so-called MR defecography) has become indispensable in the diagnosis of chronic constipation. With MR defecography, the movements of the pelvic floor and all its parts (bladder, vagina, uterus, rectum, small intestine) can be precisely tracked and displayed as a film sequence. This examination is particularly indicated for patients who are suspected of having a pelvic floor disorder or an “outlet obstruction”. An “outlet obstruction” is a constipation where the cause lies at the end of the bowel, at the exit of the bowel so to speak. Constipation is caused by a disorder of the pelvic floor if there is incorrect coordination of the pelvic floor muscles or an internal bowel prolapse.
In the latter case, the intestine is inverted into itself and thus forms a closing valve.
 In combination with MR defecography, we often also carry out a pressure measurement of the rectum or the sphincter muscle. With this examination
In combination with MR defecography, we often also carry out a pressure measurement of the rectum or the sphincter muscle. With this examination
functional disorders, i.e. disorders caused by dysregulation of the pelvic floor muscles, can also be reliably detected.
 If these examinations do not lead to a satisfactory diagnosis, a transit time measurement is necessary. In this examination, radiopaque pellets (so-called “markers”) – packed in gelatine capsules – are taken at regular intervals. If markers are still found in the intestine after 72 hours in the X-ray image, a delayed passage time can be assumed.
If these examinations do not lead to a satisfactory diagnosis, a transit time measurement is necessary. In this examination, radiopaque pellets (so-called “markers”) – packed in gelatine capsules – are taken at regular intervals. If markers are still found in the intestine after 72 hours in the X-ray image, a delayed passage time can be assumed.
How can chronic constipation be treated?
Although there is a lack of scientific data that increased fluid intake (2-3 liters per day), a high-fiber diet or plenty of exercise facilitate bowel movements, the first therapeutic approach is to change lifestyle habits to include more drinking, more fiber and more exercise. If these measures are not successful, taking stool regulators (swelling agents such as Metamucil® or Benefiber®) or laxatives can help. At our clinic, we usually use Metamucil® in combination with Transipeg forte® or Movicol®. The latter are both laxatives, which flush out the intestines to a certain extent. It is important to note here that the fear of habituation to laxatives seems unfounded, as this is not supported by any scientific data. Natural stool regulators such as wheat bran, linseed or figs can of course also be used.
If there is secondary constipation , the underlying cause of the constipation must first be remedied, for example correction of an underactive thyroid or depression.
If there is a pure dysregulation of the pelvic floor (“anismus”), relief can be achieved with physiotherapy or special pelvic floor training (“biofeedback”). However, biofeedback training is only offered at specialized centers.
In the case of primary constipation , the group with a normal transit time or passage time generally responds well to conservative measures (taking bulking agents or mild laxatives). If there is constipation with a delayed transit time, the therapy depends entirely on the patient’s symptoms. If the level of suffering is very high, the problem often has to be solved by removing the colon . Alternatively, stimulation of the pelvic floor nerves with electricity (sacral nerve stimulation or SNS) can be tried in this situation. It has been shown that this can stimulate the motor function of the entire intestine. In the case of the more common “outlet obstruction”, treatment depends on the exact cause.
Removal of the colon is the “last resort” in cases of severely reduced intestinal motor function.
If the cause of the outlet obstruction is an internal intestinal prolapse, surgical treatment must be sought. An internal prolapse is caused by a weakness in the connective tissue, which causes the rectum to tuck itself in and form a kind of blocking valve. This situation can be addressed with a new therapy known as Stapled TransAnal Rectal Resection (STARR). This method is less painful and can be performed during a 2-3 day hospitalization.
Constipation: not always a trivial problem
Chronic constipation is often a trivial problem, but not always. A prerequisite for the successful treatment of chronic constipation is a detailed assessment of the symptoms and precise knowledge of the function and anatomy of the pelvic floor. A team of different specialists (specialized surgeons, gastrointestinal specialists, radiologists and physiotherapists) is best suited to the complexity of the pelvic floor. Whenever possible, the clarification and treatment of chronic constipation should be discussed and tackled in an interdisciplinary manner, i.e. by a team of different specialists. However, the prerequisite for any therapeutic success is the patient himself or herself talking to his or her doctor about the problem of chronic constipation.
Constipation - tips for self-treatment
The treatment of constipation always depends on the underlying cause. If, for example, your lifestyle is involved, there are things you can do yourself to give your bowels “legs” again. Some tips:
- Change your diet: A poor, unhealthy diet plays a role in many health problems, including constipation. Eat more fiber-rich foods (increase your intake slowly) and drink plenty of fluids. The stool swells and the water content increases, making it softer. The fiber also increases the amount of stool. The stool exerts pressure on the sluggish bowel wall and encourages the bowel to move more. A change in diet helps some people with constipation, but not everyone.
- Fiber supplements in the form of psyllium husks, linseed and wheat bran if the change in diet has not brought sufficient success within four weeks. Drink at least one glass of water with each intake so that the fiber can swell well. Always talk to your doctor first before using fiber supplements. This is because fiber can be counterproductive in certain diseases of the rectum.
- Avoid stress: Stress can also cause bowel activity to slacken. It is best to learn a relaxation method, such as progressive muscle relaxation according to Jacobson or autogenic training. Yoga and gentle forms of exercise such as Tai Chi or Qigong can also alleviate stress. Sometimes it is enough to switch off a few stress factors in everyday life: Smartphone, PC or TV. Instead, go for a walk in the fresh air, meet up with friends or simply do what you enjoy. This can be music as well as a visit to the movies or a relaxing bath.
Laxative for constipation
Laxatives are an option if all previous measures for constipation have failed. Laxatives make the stool more fluid and fuller and thus stimulate intestinal activity. They are available as drops, coated tablets, solution, suppositories or powder. Always discuss the intake with your doctor beforehand.
There are two different types of laxatives, which differ in their mode of action:
- Intestinal stimulant laxatives: They increase the amount of water and electrolytes in the intestine and ensure that the sluggish colon moves more. Frequently used active ingredients are bisacodyl, sodium picosulphate or sennosides (preparations from the leaves and fruits of Cassia senna and Cassia angustifolia). In principle, you can also use these laxatives over a longer period of time if no diarrhea occurs. However, it is advisable to use the product for as short a period as possible until bowel movements have returned to normal.
- Water-binding laxatives: They draw water from the body into the bowel and soften the hard stool – this relieves the constipation and you can go to the toilet normally again. Examples of water-binding laxatives are Glauber’s salt and Epsom salts. Dissolve this in water and then drink the solution. However, these laxatives do not taste very pleasant. Sugars such as lactulose (can cause flatulence) and the active ingredient Magrocol (is considered to be better tolerated) are also laxatives that work on the water-binding principle. As a general rule, do not take these products over a long period of time without consulting your doctor.
Among the laxatives, the active ingredients bisacodyl, sodium picosulphate and Magrocol are the first choice.
For some, neither a change in diet, more exercise, anti-stress tips nor “normal” laxatives help. In this case, the active ingredient prucalopride is one way of relieving the blockage. The active ingredient is a so-called serotonin (5-HT4) receptor agonist and increases the movement of the intestine. It is approved for women and men with chronic constipation. The medication is only available on prescription and doctors must prescribe it.
 Examination of the pelvic floor using magnetic resonance (so-called MR defecography) has become indispensable in the diagnosis of chronic constipation. With MR defecography, the movements of the pelvic floor and all its parts (bladder, vagina, uterus, rectum, small intestine) can be precisely tracked and displayed as a film sequence. This examination is particularly indicated for patients who are suspected of having a pelvic floor disorder or an “outlet obstruction”. An “outlet obstruction” is a constipation where the cause lies at the end of the bowel, at the exit of the bowel so to speak. Constipation is caused by a disorder of the pelvic floor if there is incorrect coordination of the pelvic floor muscles or an internal bowel prolapse.
Examination of the pelvic floor using magnetic resonance (so-called MR defecography) has become indispensable in the diagnosis of chronic constipation. With MR defecography, the movements of the pelvic floor and all its parts (bladder, vagina, uterus, rectum, small intestine) can be precisely tracked and displayed as a film sequence. This examination is particularly indicated for patients who are suspected of having a pelvic floor disorder or an “outlet obstruction”. An “outlet obstruction” is a constipation where the cause lies at the end of the bowel, at the exit of the bowel so to speak. Constipation is caused by a disorder of the pelvic floor if there is incorrect coordination of the pelvic floor muscles or an internal bowel prolapse. In combination with MR defecography, we often also carry out a pressure measurement of the rectum or the sphincter muscle. With this examination
In combination with MR defecography, we often also carry out a pressure measurement of the rectum or the sphincter muscle. With this examination If these examinations do not lead to a satisfactory diagnosis, a transit time measurement is necessary. In this examination, radiopaque pellets (so-called “markers”) – packed in gelatine capsules – are taken at regular intervals. If markers are still found in the intestine after 72 hours in the X-ray image, a delayed passage time can be assumed.
If these examinations do not lead to a satisfactory diagnosis, a transit time measurement is necessary. In this examination, radiopaque pellets (so-called “markers”) – packed in gelatine capsules – are taken at regular intervals. If markers are still found in the intestine after 72 hours in the X-ray image, a delayed passage time can be assumed.