Treatment of colon cancer (colon carcinoma)
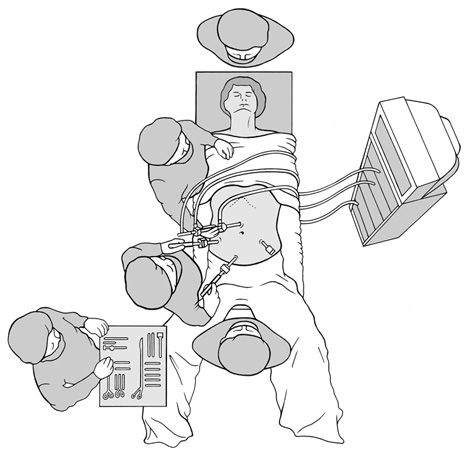
As standard, we perform minimally invasive operations, i.e. with only a few small skin incisions (so-called keyhole technique or laparoscopy). For this surgery (laparoscopic colon removal), a camera is inserted into the abdominal cavity via a small incision (2 cm) at the navel (Figures 2 and 3). With the help of other fine instruments, which are inserted through small incisions (0.5-1.5 cm) in the middle and lower abdomen, the affected section of colon can be loosened in the abdomen and then removed through an incision of around 7 to 10 cm in the middle or lower abdomen. The remaining intestinal ends are then joined together (anastomosis). After the operation, they can usually eat normally and move freely again within a few days.
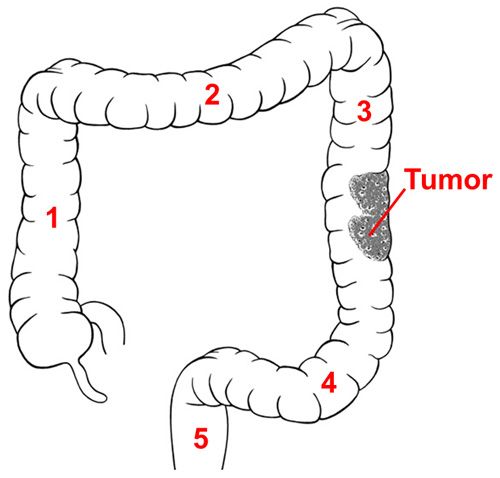
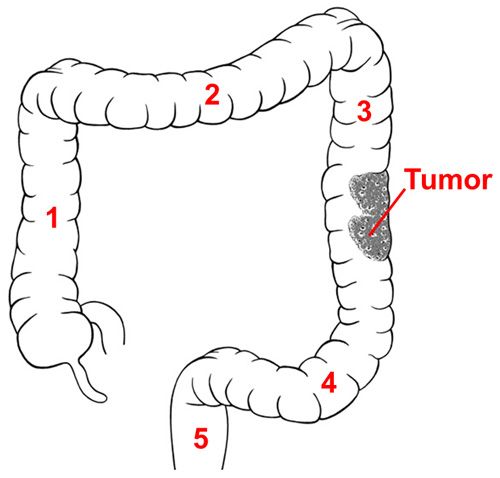
Figure 1: Schematic representation of the entire large intestine
The entire large intestine (colon)
- Ascending colon (colon ascendens)
- Transverse colon (transverse colon)
- Descending colon (descending colon)
- Rectum (sigmoid colon)
- Rectum (rectum)
- Tumor (carcinoma)
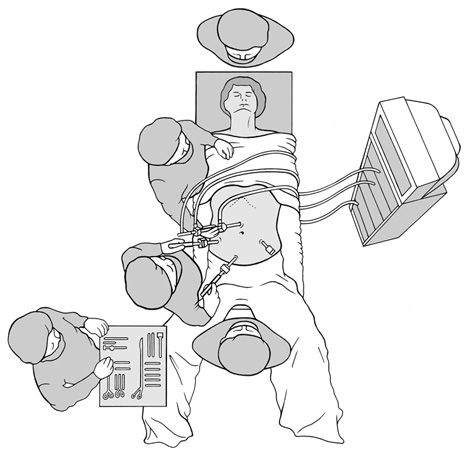
Figure 2: Laparoscopic colonic segment resection
In the meantime, a surgical robot is also often used, which, in combination with our extensive laparoscopic experience, often makes it possible to avoid a large skin incision even in more difficult cases.
The advantage of all minimally invasive techniques is that recovery after surgery is rapid and the small incisions are cosmetically inconspicuous.
We only require a longer incision in isolated cases of colon surgery. This may be necessary, for example, if a patient has already undergone several operations. The operation is then performed as an “open” procedure and the affected section of colon is removed via an incision in the middle of the abdomen (open colon resection). All techniques are equivalent in terms of radicality (comprehensive removal of the diseased tissue) and prospects of healing.

Figure 3: Working trocars and incisions during laparoscopic removal of the colon
For some patients, it is necessary to temporarily create an “artificial bowel outlet” (stoma). An artificial anus can be avoided in the vast majority of cases. Today’s techniques and materials are so good that a completely normal life is almost always possible even with a stoma. Our electricity advisory service advises and supports you in all matters.
After the operation, we promote early mobility and independence to enable you to return to your home environment quickly.
Operation information
Colon segment resection (laparoscopic/robotic) for malignant tumors
- Preparation: small enema
- Anesthesia: General anesthesia
- Operation duration: 180 to 240 minutes
- Hospitalization: 5 to 7 days
- Incapacity to work: 3 to 4 weeks
- Follow-up treatment: no suture removal, possibly chemotherapy
- Follow-up checks: Tumor follow-up, check-ups after 3, 6, 12, 24, 36, 48 and 60 months
Recommendations
Open colon segment resection for malignant tumors
- Preparation: small enema
- Anesthesia: General anesthesia
- Operation duration 120 to 180 minutes
- Hospitalization: 7 to 10 days
- Incapacity to work: 4 to 5 weeks
- Follow-up treatment: no suture removal, possibly chemotherapy
- Follow-up checks: Tumor follow-up, check-ups after 3, 6, 12, 24, 36, 48 and 60 months
Recommendations
Chemotherapy and / or radiotherapy
Depending on the stage and location of the tumor, chemotherapy and / or radiotherapy may also be necessary. For example, advanced tumors of the rectum usually require radiotherapy or a combination of radiotherapy and chemotherapy. This significantly reduces the risk of relapse. Further information on radiotherapy can be found here.
Chemotherapy is effective in most cases of colorectal cancer and nowadays causes only mild to moderate side effects. In most cases, hospitalization is not necessary. In more than half of patients with metastatic disease, the tumors shrink significantly, and in another third the growth stops.
Immunotherapy is still a new treatment. It virtually releases the “handbrake” on certain of the body’s own immune cells. These then begin to eliminate the cancer cells. So far, only tumors with certain characteristics have responded to immunotherapy, which is why this treatment is only suitable for certain patients.
Up to six out of ten people experience severe psychological stress over a short or long period of time as a result of their cancer. This stress can affect all areas of life and limit the quality of life. This is why psycho-oncology is just as much a part of the treatment plan as surgery or chemotherapy. Complementary medical treatment, nutritional therapy, exercise and other measures can usefully supplement the treatment.