Surgical techniques
Doctors usually perform the operation under general anesthesia, less frequently under spinal anesthesia. The most important surgical techniques are
Fistula splitting (fistulotomy)
During a fistulotomy, doctors cut open the anal fistula lengthwise and thus split it. In the case of fistulas that run directly under the mucous membrane, fistulotomy is unproblematic because the sphincter muscle is not affected. Fistula splitting is also an option for intersphincteric anal fistulas that only penetrate the sphincter muscle to a small extent.
Anal fistula plug (Anal Fistula Plug)
In this surgical technique, doctors insert a plug into the fistula. It consists of a tissue that comes from the small intestine of pigs. The cone fills the anal fistula completely. Doctors attach the pin to the inner fistula opening to prevent it from slipping out. Over time, the body’s own cells grow into the cone and close the fistula. The fabric material from pigs is considered safe. However, the Anal Fistula Plug is not suitable if you have an intolerance to pork egg white.
Most patients do not feel any pain after the operation. Some people report a temporary, slight pulling sensation in the area where the cone is located. You should not lift any heavy loads for more than two weeks after the operation.
Thread insert (Seton)
Another option for treating anal fistulas is the insertion of thin stitches, so-called setons. This method has been known for a long time. Setons ensure that the secretions can continuously flow outwards. Doctors use this method before a further procedure. Setons are barely noticeable. The suture insert is also suitable for complex anal fistulas or for permanent drainage.
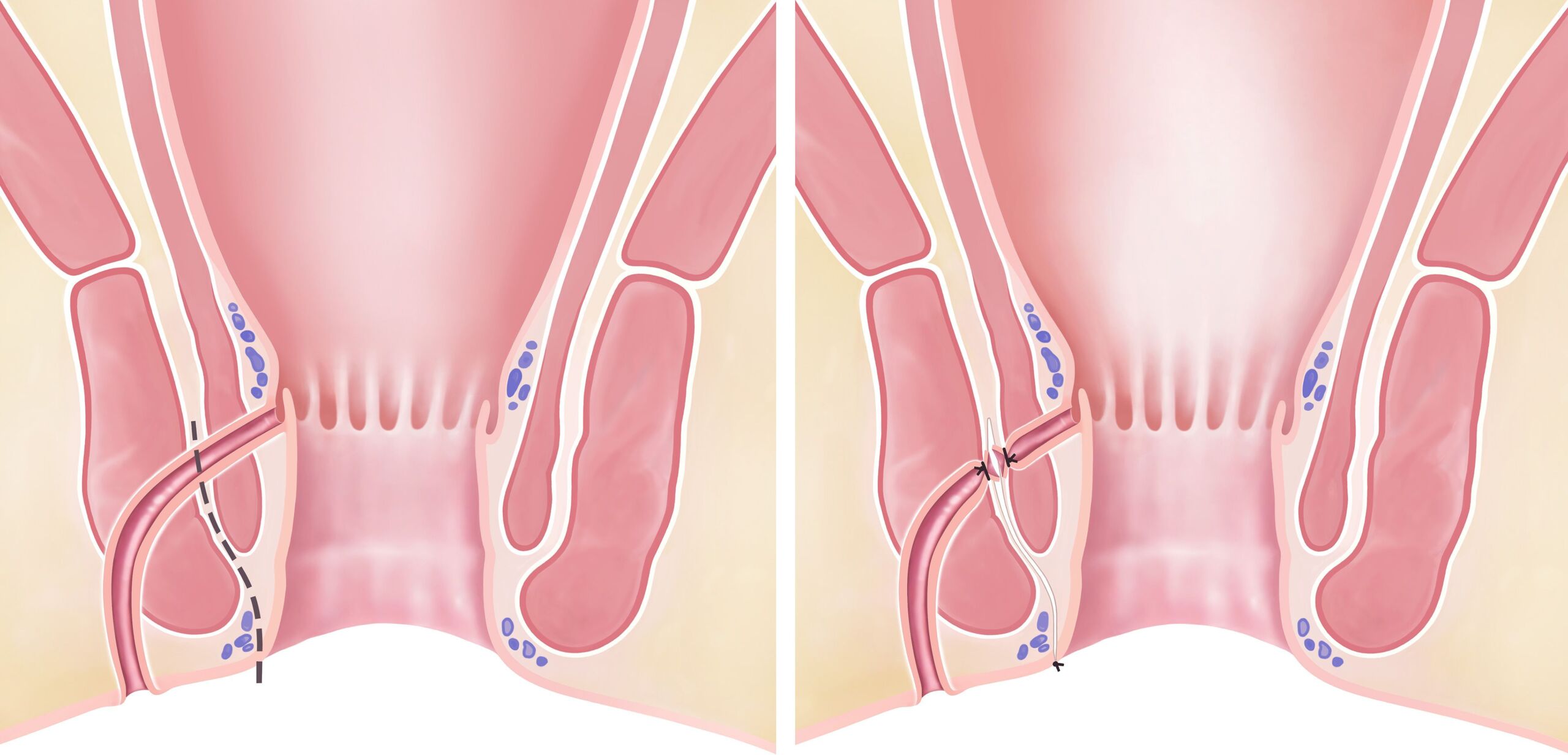
Advanced Mucosa Flap
Surgeons primarily use the so-called advanced mucosa flap for transsphincteric anal fistulas. They cut the fistula out of the tissue to the point where it penetrates the sphincter muscle. The inner opening in the intestine is sutured shut directly and additionally covered with a mucosal flap. Put simply, a cover is placed over the inner fistula opening and sutured.
But the method is not quite so easy to implement. In fact, the Advanced Mucosa Flap is a technical challenge for the doctor. She or he should therefore have sufficient experience with this surgical technique. The success rate is between 70 and 80 percent. This means that in two to three out of ten patients, the anal fistula forms again after the operation.
Fistula closure using LIFT
The abbreviation LIFT stands for LIFT. “Ligation of Intersphincteric Fistula Tract”. The surgeon exposes the fistula tract between the two sphincters, blocks it and cuts it in the middle. She or he removes the outer part of the fistula tract up to the sphincter muscle.
LIFT surgery is only suitable for anal fistulas that pass through the internal and external sphincter muscle (transsphincteric anal fistulas, type II). The LIFT-OP also achieves good results.

New therapeutic approach for the treatment of fistulas
To the press releaseGuidelines for the referral of patients for treatment with Alofisel® (darvadstrocel)
Guide d’orientation
Formulaire
Literature
(1) Panés J et al. ADMIRE CD Study Group Collaborators. Long-term Efficacy and Safety of Stem Cell Therapy (Cx601) for Complex Perianal Fistulas in Patients With Crohn’s Disease. Gastroenterology. 2018 Apr;154(5):1334-1342.
Fibrin glue
When closing the anal fistula with fibrin glue, the doctor cleans the fistula tract and then fills it with fibrin glue. However, the method can no longer stand up to today’s scientific scrutiny. Cure rates are at most 20 percent.
Laser treatment
Doctors use heat to close the fistula tract with a laser probe. Sometimes they add a sliding flap to cover them.
Video-assisted fistula treatment (VAAFT)
In this method, doctors use a special instrument (endoscope) equipped with a small camera and light source. The fistula tract is rinsed and electrically scabbed. The inner fistula opening is closed with a suture.
OTSC clip
Surgeons place an OTSC clip (Over the Scope Clip) on the inner fistula opening and close it.