Most procedures are performed as combined pancreas-kidney transplants in patients with advanced diabetic nephropathy. However, pancreas transplants are increasingly being performed after kidney transplants with equal success.
Indication
Indications for a pancreas or islet transplant are
- Age limit 50
- An individual risk-benefit assessment must be carried out before each transplantation. In general, it can be said that:
- Patients younger than 50 years of age qualify for both pancreas and islet transplantation.
- Patients who are older than 50 or have severe coronary heart disease often only qualify for an islet transplant.
Clarifications
The investigations for a combined pancreas or islet-kidney transplant include the following examinations:
- General medical examinations
- Systematic recording of all other diabetes-specific secondary diseases (retinopathy, peripheral and autonomic neuropathy)
- Reassessment and intensification of insulin therapy (possibly insulin pump)
- Clarification regarding cardiovascular diseases
- Nephrological-urological clarifications
- Exclusion of a possible infectious disease
- Exclusion of a tumor
- Immunological clarifications and tissue typing
- Clarification of the psycho-social situation and compliance
Waiting list
Once all clarifications have been completed, the treatment team discusses whether a patient can be placed on the waiting list.
Patients who receive a kidney transplant from a living donor must be transplanted in two stages.
Formal inclusion on the transplant waiting list is carried out by the Transplant Coordination of the USZ, which contacts the organ recipients regularly during the waiting period.
The timing of the transplant cannot be predicted. Depending on the blood group, the waiting time is usually two to five years until a suitable organ is available.
It is important that a patient is regularly examined and cared for by the diabetology and nephrology specialists in charge, even during the waiting period. Patients should also ensure that they can be reached at all times.
What happens during the transplant?
Pancreas transplantation
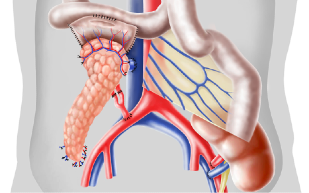
Pancreas transplantation is performed heterotopically in the abdomen, which means that this organ is also transplanted. At the University Hospital Zurich, a venous anastomosis is created between the graft, the portal vein and the superior mesenteric vein of the recipient, and an arterial anastomosis is created between the graft and the common iliac artery. The exocrine pancreatic juice is drained through the side-to-side anastomosis between the duodenum and the recipient’s jenunum.
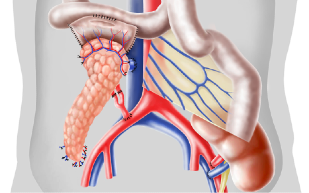
Arrangement of the organs in the abdomen and vascular connections.
Islet transplantation
After isolation and purification, the islet cells are subjected to qualitative and quantitative tests. The following conditions must be met before they can be transplanted:
- > 4000 islet equivalents per kilogram of body weight Recipient
- < than 7 ml tissue
- > 30 % purity
- > 70 % Viability
- negative Gram staining
The islet cells are infused into the recipient’s portal vein using a transplant medium. If the islet transplant is performed at the same time as the kidney transplant, the infusion takes place in the operating room. Otherwise, the radiologist punctures the portal vein transcutaneously, transhepatically and the transplanter slowly infuses the islets for 10 – 15 minutes. The islet cells enter the liver via the bloodstream and begin to function there.
Do I have to take medication?
The intake of immunosuppressants also begins with the transplant. These are drugs that suppress the rejection reaction.
For induction, i.e. immediately after transplantation, antibody therapy with basiliximab, daclizumab or ATG may be necessary. At the same time, a so-called triple therapy is initiated to prevent rejection reactions. This usually consists of:
- Calcineurin antagonist (Ciclosporin, Tacrolimus)
- Antimetabolite (mycophenolate, azathioprine)
- Steroids (prednisone)
This triple therapy is reduced and adjusted during the course of the transplant. Rapamycin or everolimus can also be used instead of calcineurin antagonists.
Steroid-free immunosuppression with Tacrolimus and Rapamun is used for islet transplantation.
How will the recipient be looked after?
In most cases, the transplant recipient can leave the hospital after seven to ten days. Subsequent outpatient care is aimed at monitoring possible rejection reactions, side effects of the immunosuppressants or the occurrence of infections.
For the time being, further follow-up care will be closely monitored in the Clinic for Endocrinology, Diabetology and Clinical Nutritional Counseling and in the Clinic for Nephrology at the University Hospital Zurich. Up to the third month weekly to fortnightly, then once a month and later once or twice a year.
After six to twelve months, the patient can be transferred back to their referring nephrologist and cared for together with them.
Life after the transplant?
After a successful pancreas or islet kidney transplant, the quality of life of most patients is described as very good. Many of them are fully able to work again and take an active part in life.
The success of the transplant is based on the following three main points:
- Regular check-ups with a diabetologist and nephrologist
- Development of good self-observation
- Regular and disciplined intake of immunosuppressive medication
What are the results?
Combined pancreas and islet transplants are now showing very good results.
With a successful combined pancreas or islet transplant, freedom from dialysis can be achieved and, with a pancreas transplant, 80 – 90 % insulin independence.
In patients with a combined islet transplant, the aim is to achieve good blood glucose control (HbA1c ~ 6 %) without severe hypoglycemia.
If this goal is not achieved, the transplantation of the islet cells can be repeated. Insulin independence can also be achieved with an islet transplant, but this is not the rule (partly due to a lack of donors). 80% of patients have their own endogenous insulin secretion after islet transplantation.
Patients are more independent again and their quality of life has improved many times over. Many of the patients are fully able to work again after the transplant.
The success of the combined transplantation depends on many factors. One of the most important factors influencing the survival of transplants is the recipient’s immune response to the donor’s tissue antigens.