Indication and contraindication
Patients with advanced renal insufficiency or renal insufficiency requiring dialysis can be transplanted due to:
- Hypertensive damage to the kidneys
- Diabetic nephropathy
- Chronic glomerulonephritis
- Polycystic kidney disease
- Chronic pyelonephritis
- Chronic interstitial nephritis
The following concomitant diseases or complications are considered contraindications for a kidney transplant:
- Tumor diseases
- Chronic infections
- advanced heart disease
- Severe liver damage
- Poor compliance and addiction problems
Clarifications
The clarifications for kidney transplantation include the following examinations of the recipient:
- General medical examinations
- Clarification regarding cardiovascular diseases
- Nephrological-urological clarifications
- Exclusion of a possible infection situation
- Exclusion of a tumor
- Immunological clarifications and tissue typing
- Clarification of the psycho-social situation and compliance
- Evaluation of the possibility of living kidney donation
In most cases, the necessary investigations can be carried out by the nephrologist or the family doctor.
Waiting list
Once all clarifications have been completed, the kidney transplant team discusses whether a patient can be placed on the waiting list. Patients who receive a kidney transplant through a living donation can be transplanted without a waiting period.
Formal inclusion on the kidney transplant waiting list is carried out by the Transplant Coordination of the USZ. The timing of the kidney transplant cannot be predicted. Depending on the blood group, the waiting time is usually two to five years until a suitable organ is available.
It is important that a patient is regularly examined and cared for by the nephrologist in charge, even during the waiting period. Patients should also ensure that they can be reached at all times. Nephrology specialists provide regular feedback on the patient’s condition and maintain close contact with the TPLZ.
Opportunities and risks?
- For many patients with advanced kidney disease, kidney transplantation offers the only chance of a cure. Of the patients transplanted at our center, over 90% are still alive after five years. This means that the chances of survival after a transplant are much better than without.
- However, not only are the chances of survival better, but the quality of life often improves dramatically after a transplant.
- However, kidney transplantation is a major and complex operation, so there is also a small risk (5 – 10 %) of dying as a result of the transplant.
What happens during a transplant?
The kidney transplant is performed under general anesthesia and takes about two to four hours. As a rule, only one kidney is transplanted. It is implanted in the right or left lower abdomen. Normally, the patient’s own kidneys are left in place. They may only have to be removed in the case of special clinical pictures.
A 15 – 25 cm long incision is made for a kidney transplant. During the operation, the blood vessels of the donor kidney are connected to the recipient’s pelvic vessels and the ureter is implanted into the bladder. The abdomen is then closed again.
Do I have to take medication?
The intake of immunosuppressants also begins with the transplant. These are drugs that suppress the rejection reaction.
Nursing consultation
The kidney transplant care consultation offers patients and their relatives continuous support after a kidney transplant.
How is the kidney recipient cared for after the transplant?
In most cases, the transplant recipient can leave the hospital after seven to ten days. For the time being, further outpatient follow-up care will be provided at the Nephrology Clinic of the University Hospital Zurich. After six to twelve months, the patient is referred back to the referring nephrologist and cared for together from then on.
Initial aftercare is as follows:
- In the first 2 weeks after transplantation: twice a week.
- Up to the third month: weekly to fortnightly.
- After that: Once a month.
- In the long term, kidney transplant patients are checked once or twice a year at the transplant center.
The aims of aftercare are
- To detect and treat a possible rejection reaction in good time.
- To adjust the immunosuppressants, record their side effects and adjust the therapy if necessary.
- Monitor the possible occurrence of infections.
Rejection and immunosuppression
The body’s immune system immediately recognizes foreign tissue and reacts with defensive reactions that can lead to the loss of a foreign organ. These immune reactions are suppressed by medication, but if a rejection reaction occurs despite these so-called immunosuppressants, special treatment must be initiated.
For induction, i.e. immediately after transplantation, antibody therapy with basiliximab, daclizumab or ATG may be necessary. At the same time, a so-called triple therapy is initiated to prevent rejection reactions. This usually consists of:
- Calcineurin antagonist (Ciclosporin, Tacrolimus)
- Antimetabolite (mycophenolate, azathioprine)
- Steroids (prednisone)
This triple therapy is reduced and adjusted during the course of the transplant. Rapamycin or everolimus can also be used instead of calcineurin antagonists.
We distinguish between acute and chronic rejections.
Symptoms of an acute rejection reaction can include
- Decrease in urine output
- Weight gain
- Fever and exhaustion
- Pain or feeling of pressure in the transplant area
- Increase in kidney values in the blood (urea, creatinine)
If you notice such symptoms after your stay in hospital, you should contact the team treating you so that the necessary investigations and treatment can be initiated.
Life after the transplant
The success of a kidney transplant is based on the following three main points:
- Regular check-ups with a nephrologist
- Development of good self-observation
- Regular and disciplined intake of immunosuppressive medication
After a successful kidney transplant, most patients describe their quality of life as very good. Many of them are fully able to work again and take an active part in life once more. After a successful kidney transplant, the quality of life of most patients is clearly improved.
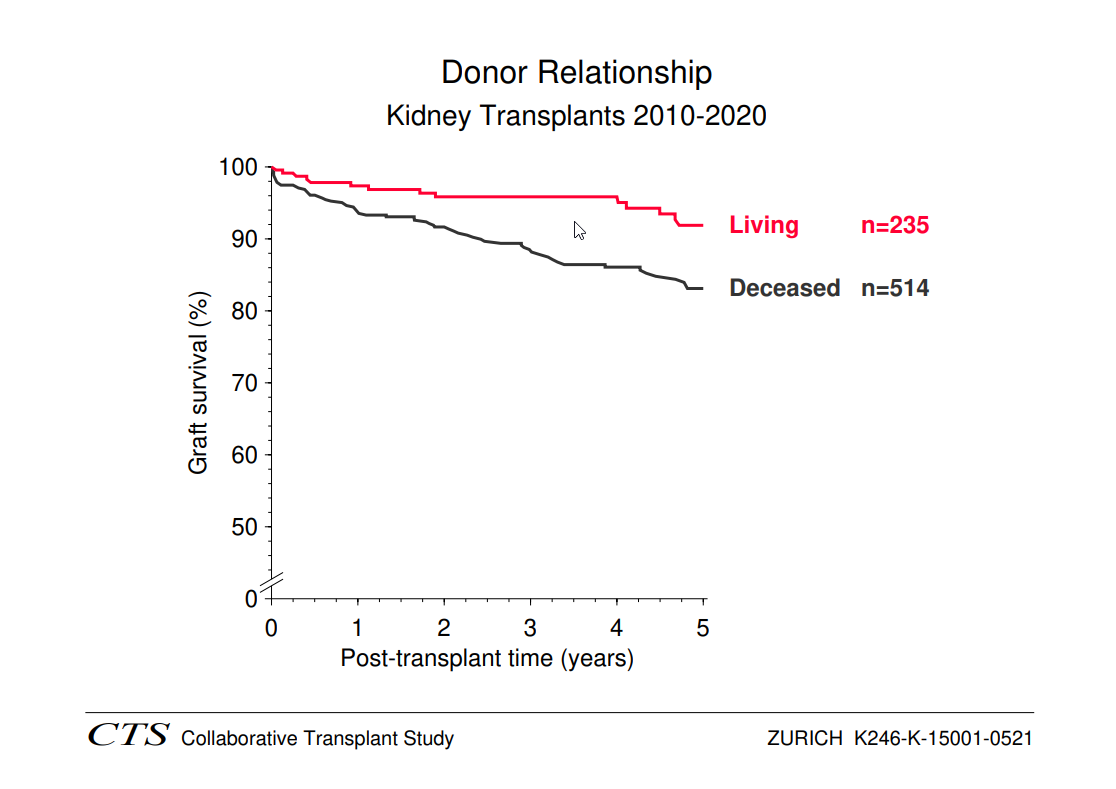
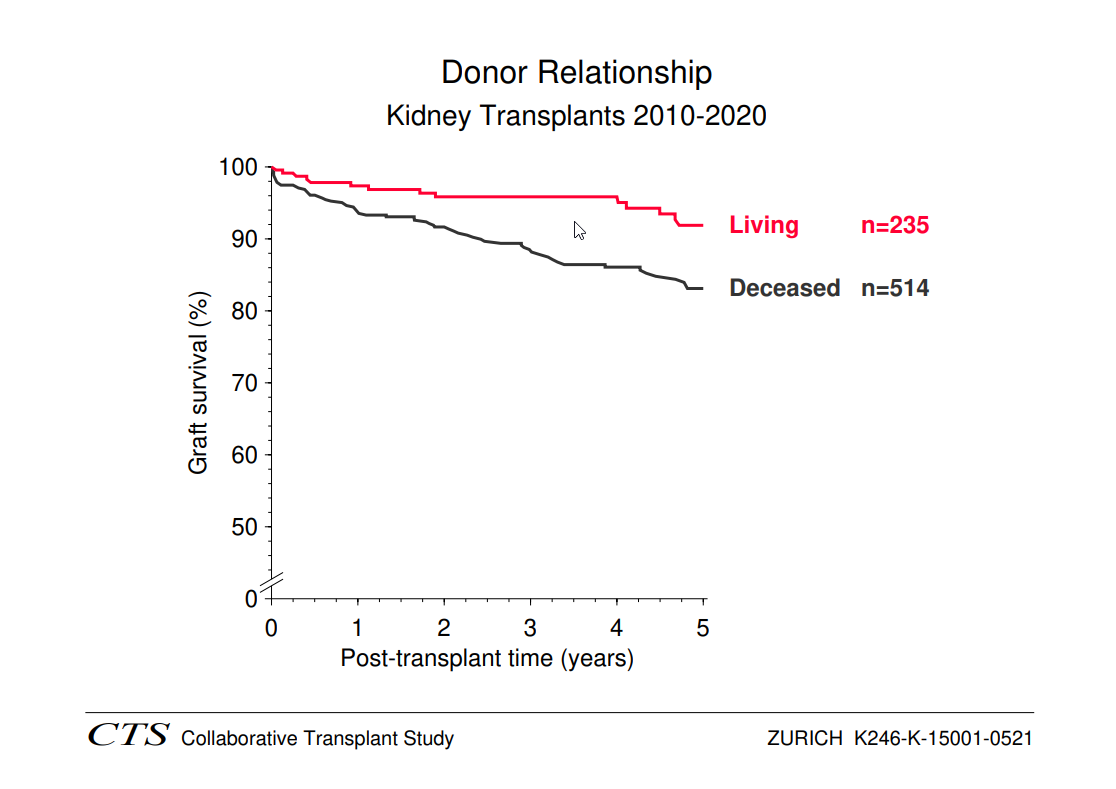
What are the results?
With a successful kidney transplant, freedom from dialysis can be achieved. Patients are more independent again and their quality of life has improved many times over. Many of the patients are fully able to work again after the transplant. Current graft survival rates are over 90% one year after transplantation and around 65% after eight years.
The so-called 1-year survival rate of a transplanted kidney is currently around 90 %. Due to chronic rejection reactions, around 40% of transplants lose their function over the course of ten years. Further kidney transplants are possible in most cases.
The graphic below impressively illustrates the very good results of kidney transplantation today.