The University Hospital Zurich began carrying out heart transplants as early as 1969, but, like the rest of the world, experienced uncontrollable rejection and infection. For this reason, the University Hospital Zurich was the first center in Switzerland to start performing heart transplants again in 1985. Subsequently, heart transplants were also carried out in Lausanne, Geneva and later in Bern and Basel. There are currently 3 centers in Switzerland: Lausanne, Bern and Zurich. By the end of 2020, a total of 497 heart transplants had been performed in Zurich. Just as important as surgery is the lifelong, individualized care of patients after transplantation.
Today, mechanical support systems also play an important role in the treatment of advanced heart failure. Heart transplantation is considered one of several options in a comprehensive range of treatment concepts for heart failure. In order to do justice to this complexity, the University Heart Center was founded at the USZ so that all patients can receive interdisciplinary care according to their needs.
Indication and contraindication
Heart failure is a serious disease that is still underestimated in terms of its frequency and severity. Thanks to important advances in therapy, the chances of survival have improved in recent years. Despite this, many people still reach the stage of severe chronic heart failure. Once the options with medication and special pacemakers have been exhausted, the last alternative is a heart transplant. It is an established and very effective therapeutic option that can return patients to normal performance and quality of life. However, due to the shortage of organs, this form of therapy only benefits (too) few patients.
A heart transplant may be considered in the following circumstances:
Any form of severe heart disease in which severe symptoms (shortness of breath, reduced exercise capacity, heart pain, arrhythmia) persist despite the full use of comprehensive therapies and life expectancy is severely restricted by the disease. Objective parameters, such as a restricted ejection fraction of the heart, exercise capacity measured by stress test and cardiac output determined by cardiac catheterization, help to find suitable patients. Affected patients must want the transplant and be motivated and positive about it, and support from relatives is also extremely important.
Are there patients who are not eligible for a heart transplant?
Yes, older patients in particular with many concomitant diseases may not be eligible as recipients, as the risk of the operation would be too high or concomitant diseases would be exacerbated by lifelong immunosuppression. For this reason, patients are thoroughly examined during a short hospitalization before a possible transplant. This involves checking whether, for example, a hidden tumor, another serious systemic disease, a severe lung or liver condition, an addiction or an uncontrollable infection make a transplant impossible.
Waiting list
Once all the clarifications have been completed, the heart transplant team and the patient discuss the options together. If the patient is suitable, he or she can be placed on the national waiting list for a transplant. The duration of the waiting time varies greatly. The donor organs are provided by deceased organ donors. In Switzerland, these are registered via Swisstransplant and allocated to recipients in accordance with Swiss guidelines.
Even while on the waiting list, patients receive very close care from the heart failure team.
What happens during the transplant?
The decisive factors for the successful transplantation of a foreign heart are the matching blood group and the similar weight and size of the donor and recipient.
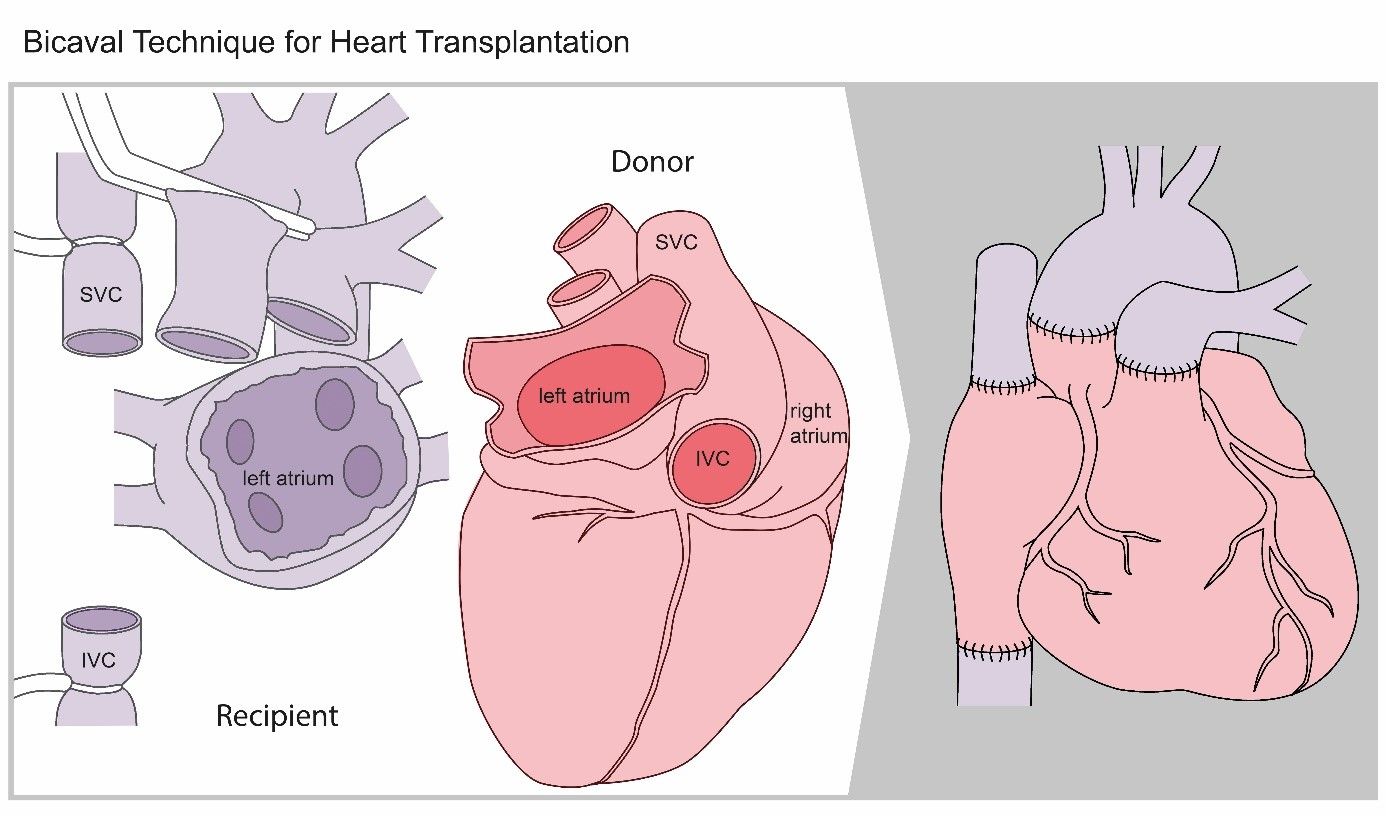
A heart transplant is performed under general anesthesia. It takes about four to six hours: the sternum is opened, the blood circulation is connected to the heart-lung machine, the patient’s heart is removed and replaced by the donor’s heart.
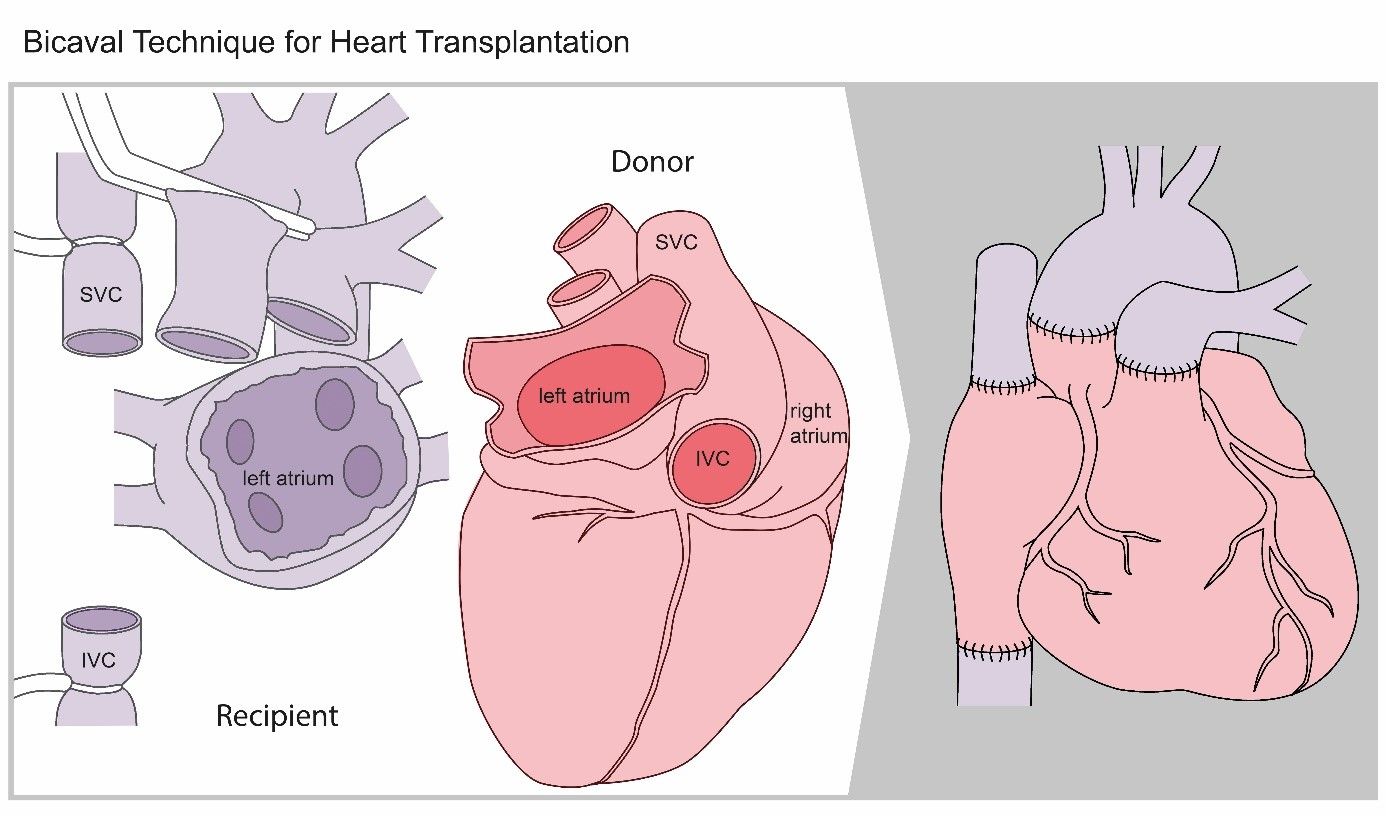
Operation sketch
At the end of the operation, the chest is closed with wires. The patient is then transferred to the intensive care unit.
Once the heart, lung and circulatory situation is stable, the patient is weaned off the ventilator. As soon as the patient’s state of health permits, he or she is transferred to the normal ward. This is followed by a 3-week rehabilitation phase.
Do I have to take medication?
The immune system, which normally protects the body from viruses and bacteria, is also able to distinguish foreign tissue from the body’s own tissue. The immune system will recognize the new heart as “foreign” and try to fight it. This defensive reaction, known as “rejection”, can be suppressed by a combination of different drugs (known as immunosuppressants). These must be taken for life.
How is the recipient looked after?
Intensive and highly specialized care and aftercare with constant monitoring with regard to rejection reactions and infections is necessary for the rest of the patient’s life.
After the transplant, follow-up care takes place in the transplant outpatient clinic by experienced nursing staff and specialized cardiologists at the USZ and in close cooperation with the family doctor, the referring cardiologist and the cardiac surgeons in the clinic.
Patients and their relatives take on an active role in self-management after transplantation following comprehensive training and support from specialists in various disciplines.
Conscientious intake of medication, daily monitoring of symptoms and timely contact with the treatment team are very important and can contribute greatly to the success of the transplant.
Rejection and immunosuppression
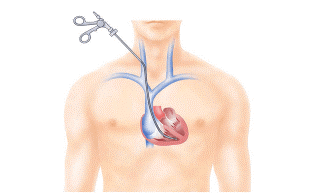
If a rejection reaction occurs despite taking immunosuppressants, a treatment specifically adapted to the situation must be initiated. A rejection reaction often does not lead to symptoms. For this reason, tissue samples must be taken from the right heart at regular intervals (so-called endomyocardial biopsies) (see below), which are examined for a rejection reaction. A first heart muscle biopsy is required approximately one week after transplantation. In the early phase after transplantation, i.e. in the first few months, heart muscle biopsies are performed at regular intervals of one to four weeks. Later, biopsies are usually only necessary every 6 months or not at all.
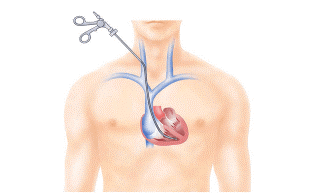
Sketch of heart muscle biopsy
Life after the transplant
The prognosis depends crucially on close cooperation between the patient and the treating team. Three main factors determine the course of the disease:
- Rejection reactions on the transplanted organ,
- Changes in the body that can be caused by immunosuppressive therapy,
- and general, transplant-independent diseases (normal ageing).
The prognosis is very good. Six months after the operation, most patients can lead a relatively normal life again.