Diagnostics
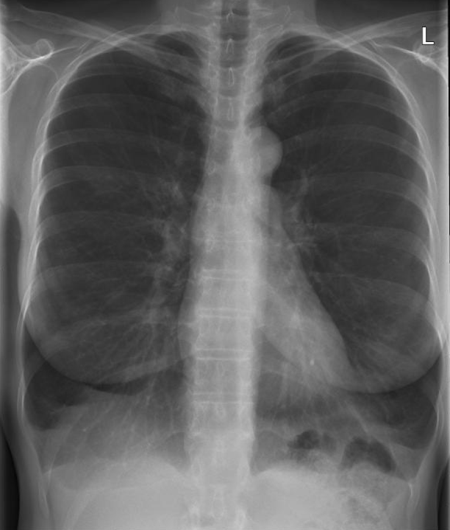
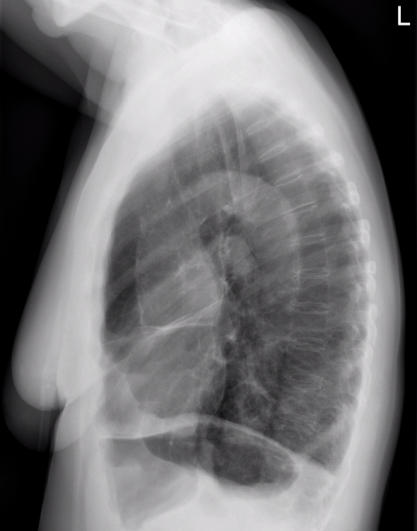
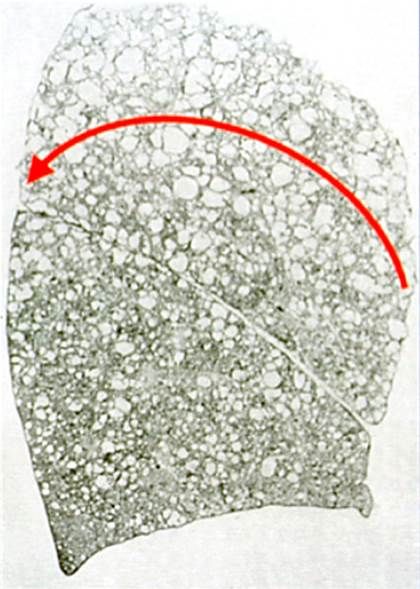
COPD is diagnosed in patients with shortness of breath, chronic cough, with or without sputum and airway obstruction in the lung function test. This usually results in emphysema (Figure 1), which shows typical signs in the overview X-ray and computer tomogram (Figure 2).
Basic diagnostics include an X-ray overview of the chest. In advanced disease, there are signs of pulmonary hyperinflation (e.g. low diaphragmatic domes, wide spaces between the ribs, widened space behind the sternum).
The computer tomography of the lungs shows the destroyed blister-like lung areas. In addition, the most damaged lung areas (= red fields) can be displayed using a color-coded representation.
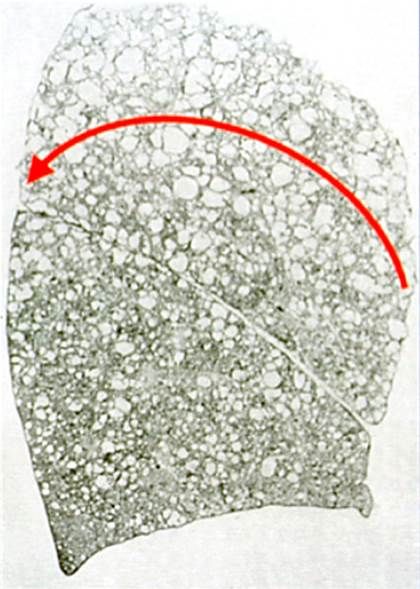
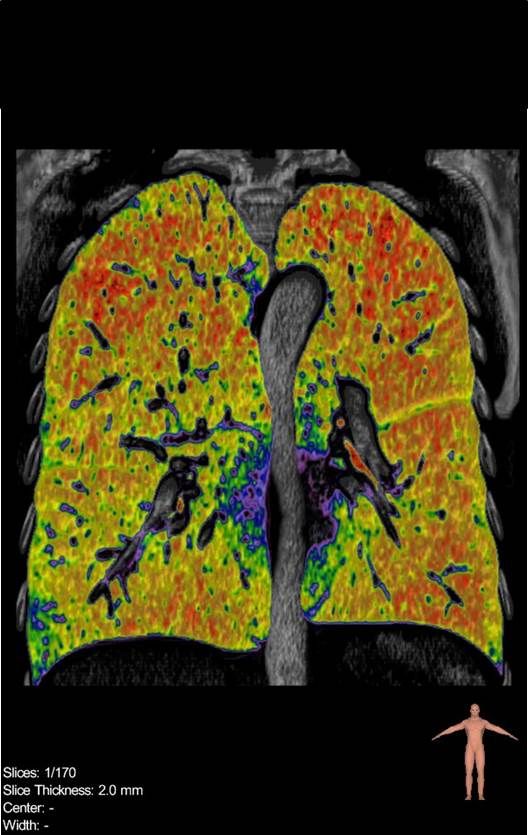
Figure 3: Removal of the most severely damaged parts of the lung.
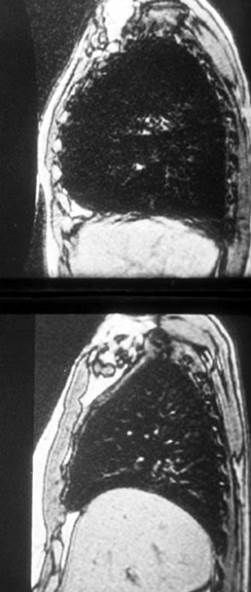
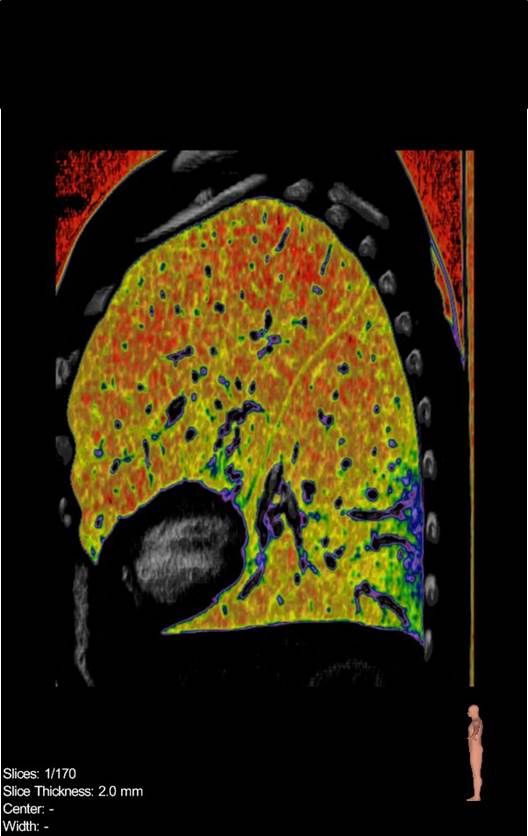
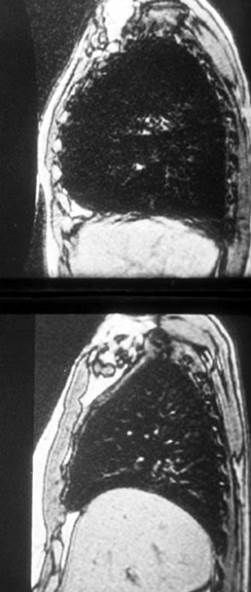
Figure 4: Lateral image before (top) and after (bottom) LVRS.
Treatment
Stopping smoking immediately is the most important measure!
Drug therapy with so-called bronchodilators, i.e. drugs to dilate the bronchial tubes, as well as anti-inflammatory drugs (steroids) and pulmonary rehabilitation (an exercise program aimed at improving performance) can reduce symptoms and stabilize the course of the disease. In advanced stages, oxygen helps to reduce breathlessness and prolong life expectancy. In this situation, two surgical procedures have been established as treatment: lung volume reduction surgery (LVRS) and/or lung transplantation (TPL).
In lung volume reduction surgery (LVRS), the most damaged parts of the lung are resected so that the oversized lung is reduced to normal size (Figure 3). In advanced emphysema, the lungs are much too large for the chest and push the most important respiratory muscle, the diaphragm, downwards so that it no longer has any function. The lung reduced to normal size allows diaphragmatic function to be restored and respiratory mechanics to be normalized again (Figure 4). The removal of the most over-inflated and destroyed, non-functional areas of the lungs also enables the development of compressed, still functional lung areas.
The most important inclusion criteria for surgical lung volume reduction are pronounced shortness of breath due to empyhsema and significant overinflation of the lungs, recognizable by the patient’s respiratory mechanics and in the pulmonary function test. The most important additional examination is the computer tomogram of the lungs, which allows the destruction of the lungs to be localized. At many centers, only patients with heterogeneous emphysema are operated on. Years ago, however, our research team was the first group worldwide to show in a large group that selected patients with homogeneous emphysema can also benefit from the procedure, with the maximum effect being measurable after six months.
The results of volume reduction are extremely good in selected patients, and they have a better quality of life. Their life expectancy also increases due to improved breathing. The maximum functional improvement is achieved three to six months after the operation. Positive effects can still be seen in many patients four to five years after the operation. In LVRS, surgery is usually performed using thoracoscopy (camera technology via three access points). The procedure is performed under general anesthesia with one-lung ventilation and can be performed on one or both sides.
Lung transplantation (TPL)
Pulmonary emphysema is the most common indication for unilateral or bilateral lung transplantation and is used in younger patients under the age of 60 who have exhausted their treatment options. It is very complex, requires lifelong medication and consistent regular follow-up checks.