Ovarian stimulation, egg retrieval, embryo cultivation, embryo transfer and cryopreservation of fertilized eggs or embryos that are not immediately transferred are the same for in vitro fertilization (IVF ) and ICSI.
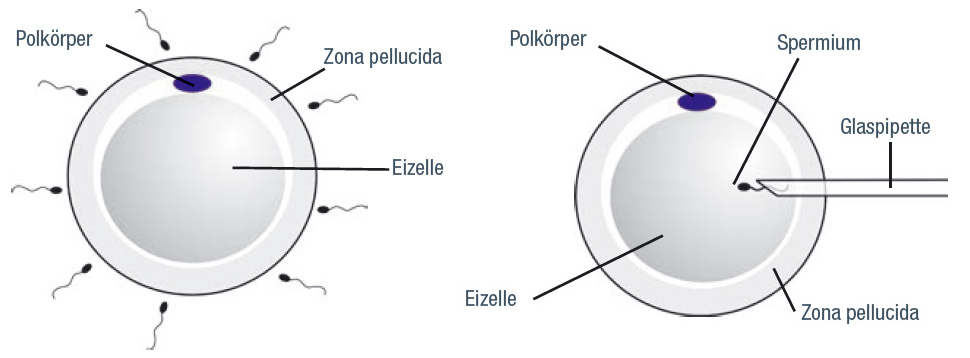
Only the fertilization of the egg cell differs from IVF as follows: In contrast to IVF, where a group of sperm directly fertilizes the egg cell (see illustration on the left), in ICSI we insert a single sperm directly into the egg cell using a very fine glass pipette (see illustration on the right).
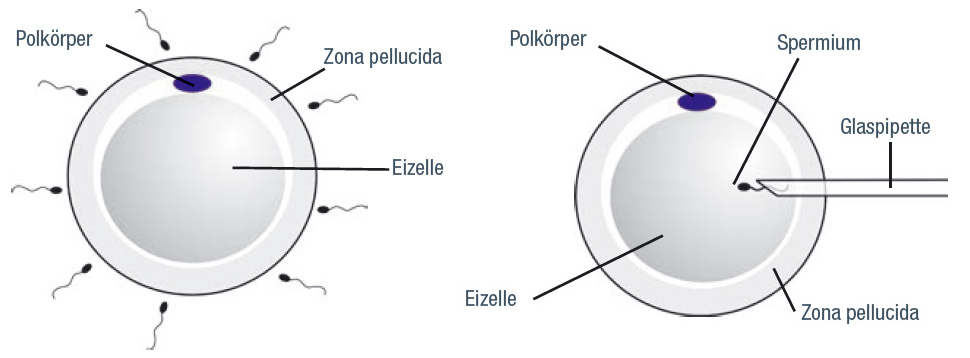
Left: IVF, right: ICSI
At our center, we are able to fulfill the wish for a baby for seven out of 10 couples, which is above average. However, this may require several treatment cycles. We would be happy to inform you about your individual chances of success during a consultation.
ICSI treatment is very easy to plan, so you can coordinate the dates with your commitments in advance. The more intensive phase lasts approx. 2-2 1/2 weeks.
You can find an overview of the ICSI treatment procedure in our information sheet.
The basic requirements for fertility treatment can be found in the FAQ of the fertility center.
Step 1: Ovarian stimulation
When preparing for the stimulation treatment, we use an ultrasound check to ensure that the conditions for successful treatment are met. At this point, you have often already started the two to three-week hormonal pre-treatment, which is well tolerated except for possible tiredness and irritability. Pre-treatment serves to optimize the subsequent maturation process of the egg cells.
To stimulate the ovaries, we use messenger substances to the ovaries. Oestrogen is produced by the maturing follicles themselves. Ovarian stimulation takes the form of daily injections, which you or your partner can easily administer yourself. We will of course instruct you on how to administer these injections.
To prevent premature ovulation, administer a so-called GnRH agonist (e.g. Decapeptyl®) or GnRH antagonist (e.g. Orgalutran®) in addition to the stimulation preparation.
The dosage of the medication is determined by the estrogen levels measured in the blood. We monitor the growth of the maturing follicles using ultrasound examinations at defined times during the stimulation process. This allows us to find the most favorable time to obtain an optimal number of mature eggs that are capable of fertilization.
As soon as the hormone and ultrasound findings have reached the required values (usually between the 9th and 13th day of stimulation), we trigger the final egg maturation and ovulation with a further injection (HCG Ovitrelle or GnRH agonist Decapeptyl®) as the last step in preparation for egg retrieval.
At each visit, we discuss the next step so that you are well informed at all times and we work together to achieve your goal.
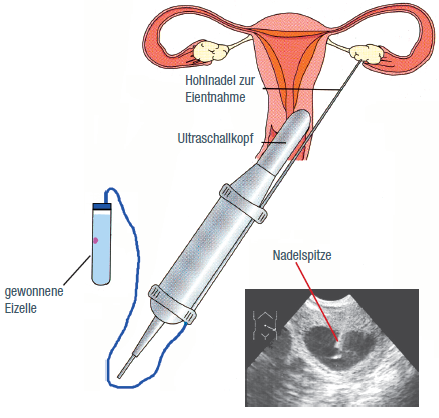
Step 2: Oocyte retrieval
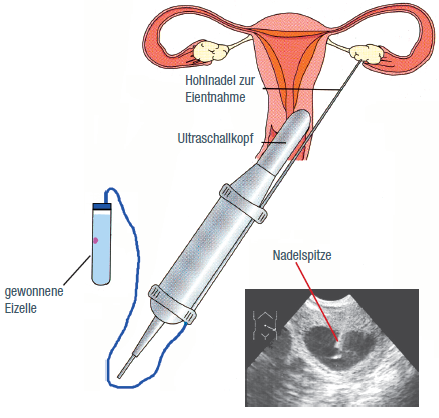
Two days after the last injection, shortly before ovulation, we puncture the follicles (follicular puncture) so that we can retrieve the mature and thus fertilizable eggs.
Follicular puncture is performed on an outpatient basis and under ultrasound guidance. The eggs and follicular fluid are aspirated from the ovaries through the vagina using a fine hollow needle. The short procedure in our operating room takes 10 – 15 minutes and, depending on your wishes and medical requirements, is performed either under a brief anesthetic or awake with a painkiller and relaxation medication. You can leave the hospital one to two hours after the procedure following a brief information session, but you are not allowed to drive a motor vehicle on this day.
Step 3: Insemination of the egg cells
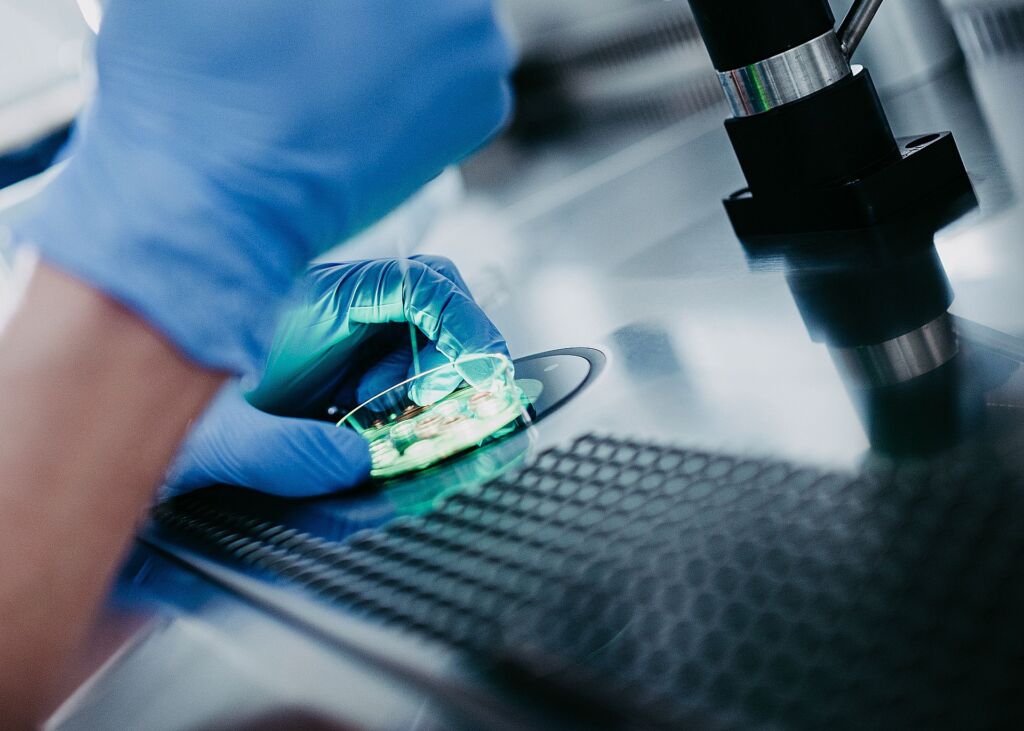
While the eggs are still being retrieved, the embryologist examines whether there are any eggs in the aspirated follicular fluid in the laboratory directly next to the operating room. All egg cells are placed in a special culture medium and rest until fertilization under ideal conditions for further development into embryos.
The ejaculate obtained after egg retrieval is prepared in the laboratory(sperm processing). The sperm that we need for ICSI usually comes from the ejaculate. If no sperm are found, a specialist urologist can remove a small piece of tissue from the testicle using a small surgical procedure. Very often we can obtain sperm from this (testicular sperm extraction, TESE), which we then use for ICSI.
The eggs are inseminated as described above.
Step 4: Embryo cultivation
The eggs are then cultivated in an incubator for two to five days under conditions that closely resemble those in nature. Fertilization should take place within 16 – 18 hours after insemination. After 40 – 64 hours, the embryos should show 2 or 3 cell divisions, i.e. two to eight cells. At this point you are ready for a transfer into the uterine cavity.
Especially when a large number of mature eggs are involved and if pre-implantation genetic diagnosis (PGD) is planned, we cultivate the embryos until the embryonic stage. 5. resp. 6th day of development, i.e. until a blastocyst. The blastocyst is similar in size to the previous days of development, but already consists of around 100 cells at this stage.
During development to the blastocyst stage, the culture is often carried out in a so-called “time lapse”, i.e. the development is monitored via a camera without disturbing the culture conditions.

Step 5: Embryo transfer (ET)
In a day 2 or day 3 embryo transfer, we transfer one or two embryos depending on the age of the expectant mother and her wishes. If a blastocyst is transferred, a blastocyst is always transferred regardless of the woman’s age. We introduce the embryos/blastocysts into the uterus in a tiny amount of culture medium using a fine, flexible catheter. When planning your treatment, we already carry out a trial transfer so that you are already familiar with this step, which is usually painless. Anesthesia is only required in exceptional cases.
Depending on the clinical situation, e.g. an increased risk of hyperstimulation syndrome, which is present in polycystic ovary syndrome (PCOS), for example, an embryo transfer may not be carried out immediately after egg retrieval but only in a later cycle.
Corpus luteum phase
From the day of egg retrieval, you will receive the natural corpus luteum hormone progesterone. This optimally prepares the uterine lining for pregnancy. You use progesterone at least until the pregnancy test, in the case of pregnancy until the 10th week of pregnancy.
Pregnancy test
Approximately 12-14 days after the embryo transfer, you will come to us for a blood pregnancy test. This not only tells us whether you are pregnant, but also gives us an initial indication of whether everything is in order with the pregnancy. If this test is positive, we will carry out a first pregnancy ultrasound check approx. 10 days later.
Step 6: Cryopreservation of embryos and blastocysts
If several fertilized eggs, embryos or blastocysts are created during the stimulation treatment, we transfer a maximum of two embryos or one blastocyst immediately afterwards. We can freeze the remaining embryos and blastocysts and store them for you for up to ten years in accordance with the Swiss Reproductive Medicine Act. Whether and how many fertilized eggs, embryos or blastocysts can be frozen varies greatly from person to person.
Frozen embryos or blastocysts can be thawed in later cycles and transferred to your uterus. With today’s techniques, almost all frozen embryos and blastocysts are intact even after thawing and, especially at our center, allow for pregnancy chances comparable to those after a transfer following stimulation treatment.
Basically, there are different times when freezing is particularly beneficial. This includes freezing directly after fertilization and freezing at the blastocyst stage.
The natural ovarian hormones estradiol and progesterone optimally prepare the uterine lining for the transfer of embryos and blastocysts. We determine the right time for the transfer by means of an ultrasound examination.
Embryos and blastocysts are only cryopreserved with your consent. The exact conditions are set out in a separate agreement.
Security
Our cryotanks are equipped with state-of-the-art safety systems and a competent team is available around the clock to deal with any emergencies. This means that your valuable embryos and blastocysts are optimally protected at all times. Being part of a proven, long-standing and solid organization like the USZ ensures that your embryos and blastocysts are available when you need them.
Organization and costs
We would be happy to inform you in a personal consultation about the possibilities and opportunities to support your desire to have children. Please ask your gynecologist to refer you. The results of any preliminary clarifications make it easier for us to provide advice tailored to your needs.
The costs of preliminary clarifications for fertility treatment are covered by health insurance.
In the case of ICSI, you are responsible for the treatment costs from the start of hormone treatment. You can expect to pay between CHF 5,000 and CHF 7,000 per treatment cycle at our center, depending on the cost. A treatment cycle includes the implementation and monitoring of hormone therapy (stimulation), egg retrieval (puncture), fertilization and cultivation of eggs and embryos (laboratory) and transfer of the embryos into the uterus (transfer). In addition, there are any costs for freezing (cryopreservation) and storing the fertilized eggs/embryos that are not directly transferred, which amount to CHF 700, and the annual storage fee of CHF 400.
We need hormones to mature the egg cells (stimulation). The additional costs for this amount to CHF 1,000 to CHF 2,000, depending on the product and the quantity of hormone required.