Diagnostics
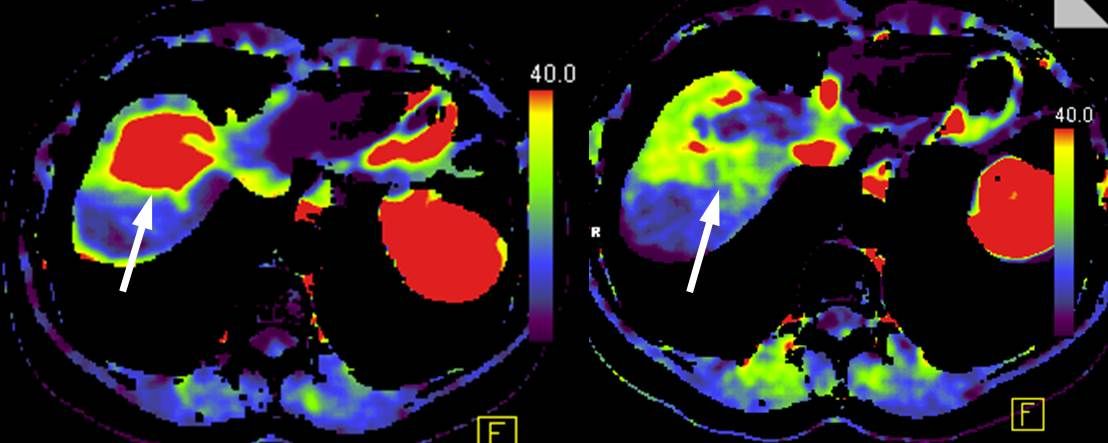
In liver diagnostics, ultrasound is used as a so-called “screening” examination. With high-resolution sonography devices and additional contrast enhancement using a contrast agent specially developed for ultrasound, small tumors can increasingly be detected. In many cases, magnetic resonance imaging (MRI), which, like ultrasound, does not require any radiation exposure, is necessary for the precise characterization of the tumour. The so-called “liver-specific” (“hepato-biliary”) contrast agent is used for the examination of liver lesions in MRI. This “liver-specific” contrast agent is absorbed by healthy liver cells 10-20 minutes after intravenous administration, while tumor cells in malignant tumors do not absorb this contrast agent or only to a small extent. With the help of this specific contrast medium information and the excellent organ contrast in the MRI, normal liver tissue or benign liver tumors can be differentiated from malignant liver tumors with a high degree of diagnostic accuracy.
In addition to the characterization of liver tumors, MRI also provides comprehensive information for planning liver surgery, such as the exact number of liver tumors, the positional relationship and exact course of the hepatic arteries, portal veins, hepatic veins and bile ducts, as well as the liver volume.
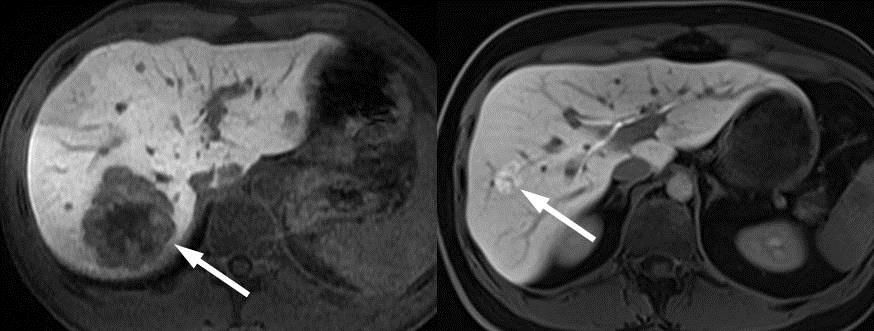
Malignant liver tumor (liver metastasis) with slight accumulation of the “liver-specific” contrast agent (left). Benign liver tumor (focal nodular hyperplasia) with strong accumulation of the “liver-specific” contrast agent (right).