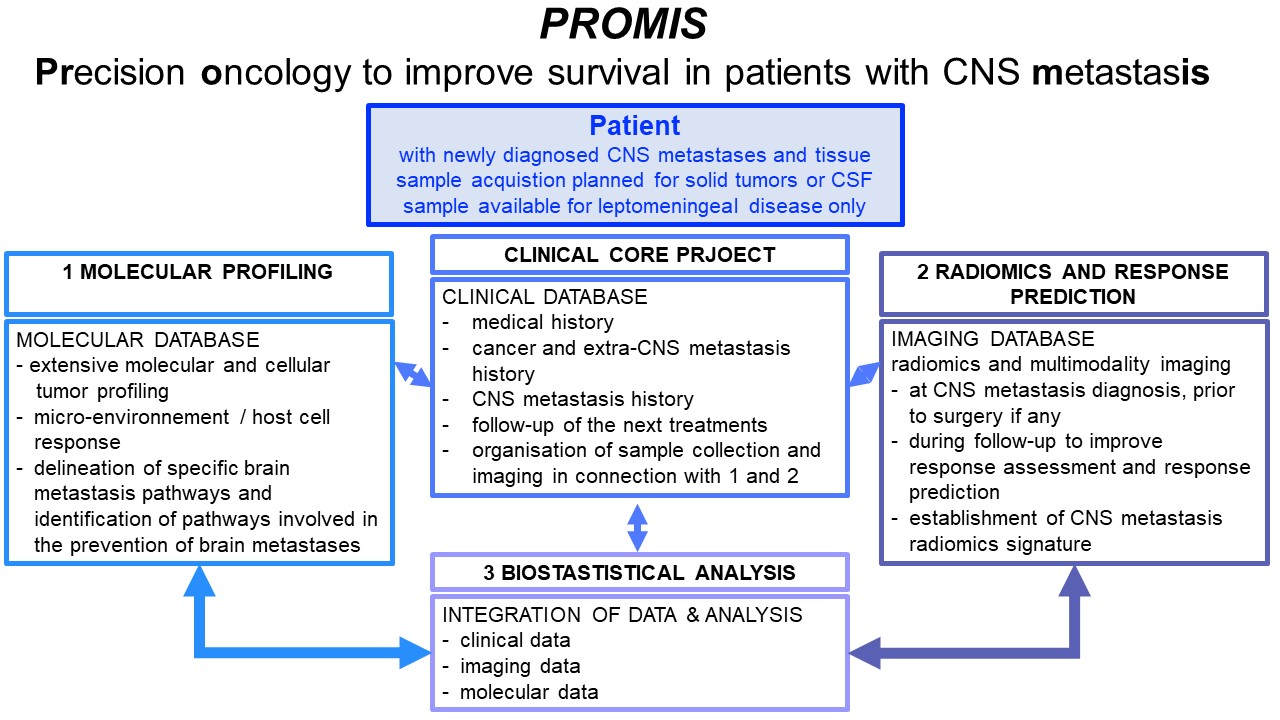
PROMIS – Precision oncology to improve survival in patients with CNS metastasis
Keywords
Brain, Cancer, Metastasis
Project Overview
Brain and leptomeningeal metastases are an emerging area of clinical and experimental research in oncology. This is due to increasingly effective therapies of solid tumors at non-central nervous system (CNS) sites and thus longer overall survival. Brain metastases may affect up to 30%, and leptomeningeal metastases up to 10%, of patients with metastatic cancer. They are a major cause of morbidity and mortality and most common in melanoma, lung, breast and kidney cancer and develop in a distinct pattern by primary tumor, e.g., much earlier in lung cancer than in other entities. Treatment includes neurosurgery, radiotherapy, and systemic and rarely intrathecal pharmacotherapy.
CNS metastases represent a challenge in diagnosis and treatment. Many clinical trials exclude patients with brain metastases and dedicated brain metastases trials are rare, systematically depriving brain metastasis patients from progress in clinical oncology, despite their poor prognosis. Moreover, with the increasing use of stereotactic radiotherapy and immunotherapy in patients with brain metastasis, assessment of response or progression based on neuroimaging has become a major challenge, but efforts at standardization of imaging for patients with brain metastases are under way.
The branched evolution of cancer has become a dominant concept in oncology with a particular focus on brain metastasis. It proposes that cancer cells seeding in different organs do not evolve randomly, but are shaped or selected for by interactions with their microenvironment (the metastatic niche). This concept has triggered studies comparing various features of brain metastases with primary tumors or metastases outside the brain preferentially in patients with lung cancer, breast cancer, and melanoma. Most studies focused on selected genes characteristic for subtypes of these tumors, e.g., hormone receptor status in breast cancer. Unbiased approaches have indicated that the changes found in brain metastases may be rather heterogeneous. These considerations support the major prediction of this project that tissue acquisition from brain metastases followed by deep molecular profiling may disclose vulnerabilities specific to brain metastases that may be amenable to targeted interventions. Moreover, decipherung the host response in the brain as opposed to metastases outside the CNS may disclose new avenues on how to best treat CNS metastasis.
The CNS Metastasis research efforts of the Comprehensive Cancer Center Zurich currently receives support from the Sophien Foundation, the Foundation for Applied Cancer Research (SAKF), the Promedica Foundation and the USZ Foundation.
Clinical Trials
Two clinical trials are now open in Zurich in the field of CNS metastasis:
ETOP 19-21 USZ-STRIKE
Immunotherapy or targeted therapy with or without stereotactic radiosurgery for patients with brain metastases from melanoma or non-small cell lung cancer
This trial is conducted under the sponsorship of ETOP and examines whether patients with newly diagnosed brain metastasis from non-small cell lung cancer or melanoma, who are candidates for systemic treatment, should receive radiosurgery upfront or at further progression. The trial was made possible by the USZ foundation.
IT-IO
Intrathecal administration of anti-PD1/anti-CTLA-4 in combination with systemic combination of anti-PD1/anti-CTLA-4 in patients with NSCLC without oncogenic driver mutation or melanoma and newly diagnosed leptomeningeal metastasis: a multicentric phase I study
This trial is a phase I trial conducted at several sites in Switzerland to explore the safety and preliminary activity of intrathecal double immune checkpoint inhibition in patients with newly diagnosed brain metastasis from non-small cell lung cancer or melanoma.
Collaboration and personalized medicine to improve quality of care and access to innovative research
Principal investigators and cooperating departments
Emilie Le Rhun, Department of Medical Oncology and Hematology, University Hospital Zurich, Emilie.Lerhun@usz.ch (Principal investigator)
Michael Weller, Department of Neurology, University Hospital Zurich, Frauenklinikstrasse 26, 8091 Zurich, Michael.weller@usz.ch
Nicolaus Andratschke, Department of Radiation Oncology, University Hospital Zurich, Rämistrasse 100, 8091 Zurich, Nicolaus.Andratschke@usz.ch
Burkhard Becher, Institute of Experimental Immunology, University of Zurich, Winterthurerstrasse 190, 8057 Zurich, becher@immunology.uzh.ch
Andrea Bink, Department of Neuroradiology, University Hospital Zurich, Frauenklinikstrasse 10, 8091 Zurich, Andrea.bink@usz.ch
Alessandra Curioni, Clinic for Medical Oncology and Hematology, University Hospital Zurich, Rämistrasse 100, 8091 Zurich, Alessandra.curioni@usz.ch
Konstantin Dedes, Department of Gynecology, University Hospital Zurich, Frauenklinikstrasse 10, 8091 Zurich, konstantin.dedes@usz.ch
Reinhard Dummer, Department of Dermatology, University Hospital Zurich, Gloriastrasse 31, 8091 Zurich, Reinhard.dummer@usz.ch
Matthias Guckenberger, Department of Radiation Oncology, University Hospital Zurich, Rämistrasse 100, 8091 Zurich, Matthias.Guckenberger@usz.ch
Michael Krauthammer, Department of Quantitative Biomedicine, University of Zurich, Schmelzbergstrasse 26, 8006 Zurich, Michael.Krauthammer@usz.ch
Mitchell Levesque, Department of Dermatology, University Hospital Zurich, Gloriastrasse 31, 8091 Zurich, Mitchell.Levesque@usz.ch
Holger Moch, Department of Pathology and Molecular Pathology, University Hospital Zurich, Schmelzbergstrasse 12, 8091 Zurich, holger.moch@usz.ch
Luca Regli, Department of Neurosurgery, University Hospital Zurich, Frauenklinikstrasse 10, 8091 Zurich, Luca.regli@usz.ch
Isabelle Schmitt-Opitz, Department of Thoracic Surgery, University Hospital Zurich, Rämistrasse 100, 8091 Zurich, Isabelle.Schmitt-Opitz@usz.ch
Tobias Weiss, Department of Neurology, Department of Neurology, University Hospital Zurich, Frauenklinikstrasse 26, 8091 Zurich, tobias.weiss@usz.ch
Andreas Wicki, Clinic for Medical Oncology and Hematology, University Hospital Zurich, Rämistrasse 100, 8091 Zurich, Andreas.Wicki@usz.ch