It has only been known for a few years that the use of certain medications, so-called antiresorptives, can sometimes lead to tissue death in the jawbone as a side effect. These cases are referred to as drug-associated osteonecrosis. Here, too, infections with germs from the oral cavity play an important role in the development. Early diagnosis is important for both osteomyelitis and drug-associated osteonecrosis of the maxilla and mandible so that treatment can begin as early as possible. Good dental and oral hygiene plays an important role in the prevention of both diseases.
Osteomyelitis and drug-related osteonecrosis (MRONJ) of the maxilla and mandible
MRONJ
Osteomyelitis of the upper and lower jaw is an inflammation of the jawbone, usually caused by an infection with bacteria from the oral cavity. Depending on the extent, osteonecrosis can develop in the further course, i.e. bone tissue in the jaw can die off.
What are osteomyelitis and drug-related osteonecrosis (MRONJ) of the maxilla and mandible?
Although osteomyelitis translates as inflammation of the bone marrow, the entire jawbone with all its layers is usually inflamed in osteomyelitis of the jaw. A distinction is made between acute and chronic forms of osteomyelitis. Chronic osteomyelitis is when the inflammation in the jaw lasts longer than four weeks. The inflammation usually develops as a result of an infection with bacteria that originate in the oral cavity and have penetrated to the jawbone.
Osteonecrosis is generally understood to be the death of bone tissue. In the upper and lower jaw, such a loss of bone tissue can also occur as a side effect of certain medications. This is also referred to as drug-associated osteonecrosis. The abbreviation MRONJ stands for the English equivalent of the term: medication-related osteonecrosis of the jaw.
Osteomyelitis and drug-related osteonecrosis (MRONJ) of the maxilla and mandible: infection is usually the cause
The mouth is full of bacteria. Under certain circumstances, they can penetrate through the teeth and periodontium to the jawbone. Fortunately, however, this happens relatively rarely. Thanks to good tissue perfusion and the immune system’s defense mechanisms, the body is normally able to ward off or keep invading germs at bay. However, if the balance shifts, for example because the number of pathogens increases, the pathogens are particularly aggressive or the immune defense is weakened, an infection of the jawbone can occur.
If there are underlying diseases that impair the immune system, this can favor osteomyelitis of the jaw. Such diseases include, for example
- Diabetes mellitus (diabetes)
- Autoimmune diseases
- Anaemia (anemia)
- Blood cancer (leukemia)
If tissue perfusion is impaired at the same time, this is an additional risk factor for the development or spread of osteomyelitis in the jaw. This is because a lack of blood flow means that the tissue is not adequately supplied with oxygen and nutrients, and the immune system’s defense cells cannot get to where they are needed. As many pathogenic germs prefer a low-oxygen environment, they can multiply and spread particularly well in poorly perfused tissue and without sufficient defense from the immune system. Certain factors can promote poor tissue perfusion and thus also osteomyelitis. These risk factors include, for example
- Smoking
- Diabetes mellitus (diabetes)
- pre-existing bone diseases (e.g. Paget’s disease, fibrous dysplasia or osteopetrosis)
Osteomyelitis usually develops in the lower jaw. This is because, compared to the upper jaw, the lower jaw is only supplied with a small amount of blood.
In most cases, osteomyelitis in the jaw is caused by an infection with germs from the oral cavity, for example as a result of gingivitis or unerupted teeth. In some cases, however, osteomyelitis also develops after fractures in the jawbone that have not been properly treated or as a result of surgical procedures in the jaw area.
Osteonecrosis as a side effect of medication
In some cases, inflammatory conditions in the jawbone develop as a result of taking certain medications, especially so-called antiresorptives. If the connection between the symptoms and the medication is not recognized at an early stage, bone death, i.e. osteonecrosis, can quickly develop. Why bone tissue loss occurs as a side effect, particularly in the jawbone, has not yet been clarified with certainty.
The group of antiresorptives includes active substances that reduce bone resorption, such as bisphosphonates or denosumab. They are prescribed for diseases that are associated with increased bone resorption, for example:
- Osteoporosis (bone loss)
- Paget’s disease
- Brittle bone disease (osteogenesis imperfecta)
- Cancer (such as plasmacytoma, multiple myeloma or metastases due to breast cancer, prostate cancer, kidney cancer or lung cancer)
There is an increased risk of drug-associated osteonecrosis of the upper and lower jaw, particularly when antiresorptives are used as part of cancer treatment. This is because the medication has to be administered in much higher doses and more frequently than in the treatment of osteoporosis, for example.
Antiresorptives interfere with bone metabolism and also impair the immune system’s defense processes in the bone. This can pave the way for infections. Unlike other bones, the jawbone has an almost direct connection to the outside world via the teeth. Its only protection is the delicate periosteum and a thin mucous membrane. This means that even minor injuries to the mucous membrane can presumably provide an entry point for germs from the oral cavity and lead to infections and inflammatory processes in the bone tissue.
Certain factors can favor such infections, such as:
- Inflammation of the gums (gingivitis)
- Inflammation of the periodontium (periodontitis)
- problematic tooth eruptions (e.g. wisdom teeth)
- Injuries to the oral mucosa (e.g. when brushing teeth, due to dentures, sharp bone edges, biting the tongue or cheek)
- Unprofessionally performed dental surgery
Osteomyelitis and drug-related osteonecrosis (MRONJ) of the maxilla and mandible: symptoms
Osteomyelitis of the jaw can cause different symptoms, depending on whether it is an acute inflammation of the jawbone or whether it has already become chronic. Chronic osteomyelitis of the jaw is when the inflammation lasts longer than four weeks.
Osteomyelitis and drug-associated osteonecrosis can be accompanied by similar symptoms. Possible symptoms include:
- Dull to severe pain in the jaw
- Soft or hard swelling of the soft tissue in the oral cavity or jaw area
- Bad breath
- Abscess formation in the jaw area
- Mouth cannot be opened normally wide
- Feeling of loose teeth in the area of inflammation
- Tubular connection from the jaw to the skin surface (so-called fistula)
- Loss of sensation in the lower lip due to sensory disturbance in the area supplied by the inferior alveolar nerve (so-called Vincent syndrome)
- Dead (necrotic) bone tissue
- Exposed jawbone
- Fractures in the jawbone without an external cause
- Sinusitis
Especially in acute osteomyelitis, swollen lymph nodes, fever (39 to 40 degrees Celsius) and a strong feeling of illness are typical.
Osteomyelitis and drug-related osteonecrosis (MRONJ) of the maxilla and mandible: diagnosis at our clinic
In order to make a diagnosis of osteomyelitis and/or drug-associated osteonecrosis of the upper and lower jaw, we first take a thorough look at the mouth and jaw area. Blood tests can show whether there are increased inflammatory values such as an increased CRP value or an increased leukocyte count (leukocytosis). Of particular interest is whether the patient is being or has been treated with medication from the group of antiresorptives.
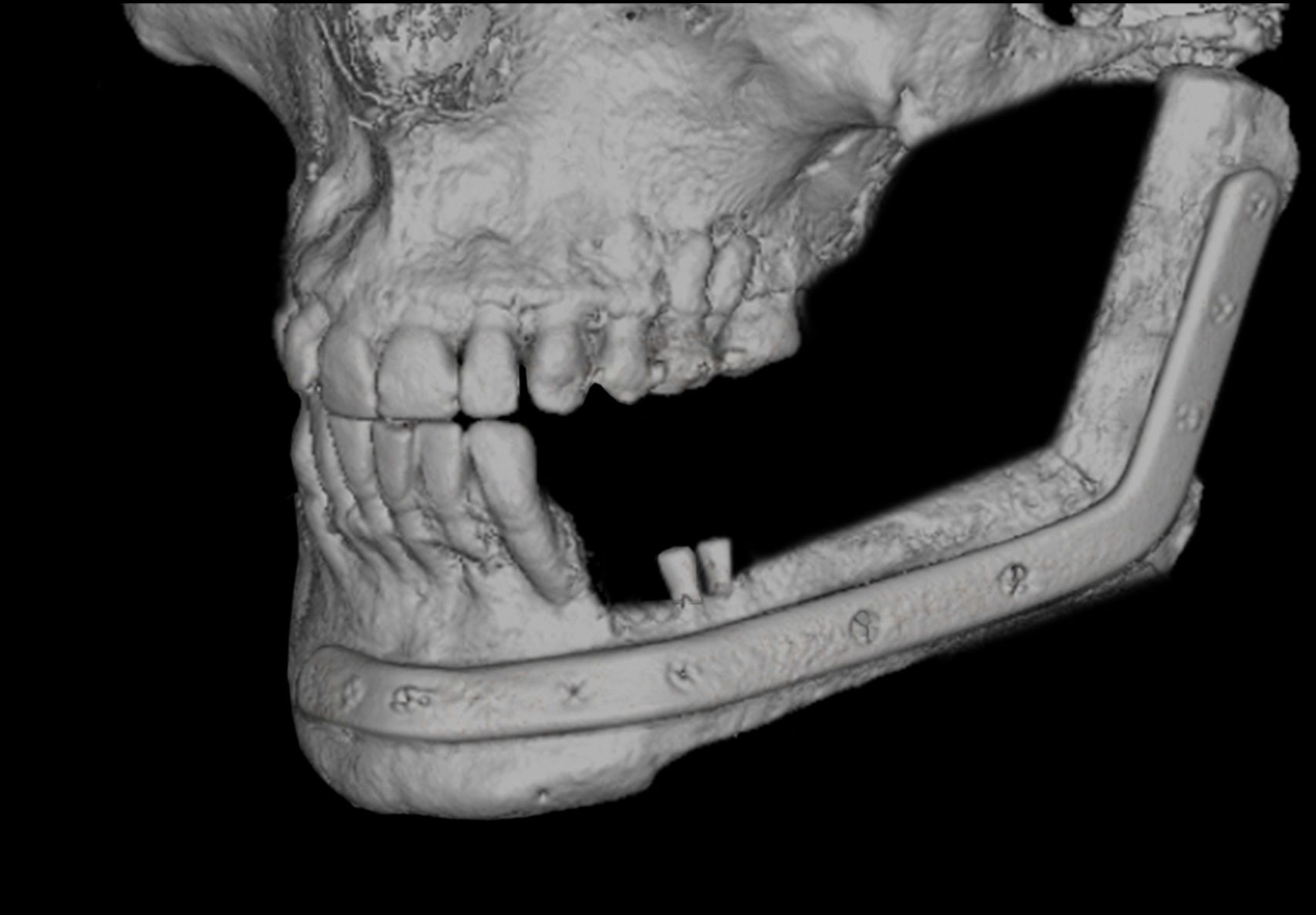
In order to gain a more precise insight into the jawbone, various imaging examinations play a role, for example:
- Panoramic tomography (orthopantomogram, OPG): semi-circular X-ray of the jaw from one ear to the other
- Digital volume tomography: three-dimensional X-ray of the jaw
- Computed tomography (CT): layer-by-layer X-ray images of the jaw
- Magneticresonance imaging (MRI): layer-by-layer images of the jaw using a strong magnetic field and radio waves
- Bone scintigraphy (SPECT/CT): nuclear medicine examination that can be used to examine bones and bone metabolism
A tissue sample (biopsy) can also show the nature of the changes in the bone tissue. This is important to rule out the possibility of cancer.
Osteomyelitis and drug-related osteonecrosis (MRONJ) of the maxilla and mandible: preventive measures
Infections caused by bacteria from the oral cavity play an important role in both osteomyelitis and drug-associated osteonecrosis in the jaw. However, these diseases can be prevented to a certain extent with optimal oral and dental hygiene. In addition to the correct brushing technique, this also includes the regular use of dental floss and attending dental check-ups.
Before starting treatment with antiresorptives, it is generally advisable to make an appointment with your dentist. This makes it possible to determine in good time what condition the teeth are in, whether there are any possible sources of infection and whether there is sufficient knowledge about how to take optimum care of the teeth. In particular, if antiresorptives are used as part of cancer treatment, it may be advisable to complete any necessary dental treatment or denture adjustments before the start of therapy.
Even during treatment with antiresorptives, patients should have regular dental check-ups (at shorter or longer intervals depending on the individual risk situation) and ensure very good oral and dental hygiene. It is also advisable to have your teeth professionally cleaned at regular intervals.
If dental procedures are necessary that may result in injuries to the mucosal covering of the jawbone, antibiotics should also be part of the treatment as a preventative measure – ideally at least the day before the procedure. The procedures should also be carried out in such a way that they offer as few opportunities as possible for bacteria to enter.