Treatment options for CTEPH
All patients should first be assessed for possible surgery (see below). This is the only truly effective therapy for CTEPH. This is due to the fact that it is primarily a “mechanical” problem that should also be resolved “mechanically”, i.e. surgically. Drug therapy should really only be carried out in cases where surgery is not possible based on the assessment of pulmonary angiography by the surgeon. Patients can also receive advice on this in the consultation hours for pulmonary hypertension.
Consultation hours for pulmonary hypertension
We offer state-of-the-art diagnostic and therapeutic procedures for patients with various forms of pulmonary hypertension.
Pulmonary endarterectomy (PEA)
An operation has been available for over 30 years which, in the best case, can lead to a cure for pulmonary hypertension. This is known as pulmonary endarterectomy (PEA), formerly also referred to as pulmonary “thrombendarterectomy”. The word “thromb” is no longer used today because the pulmonary arteries in CTEPH are no longer blocked by embolisms (clots), but have become scarred over time, so that there are mainly changes in the vessel walls.
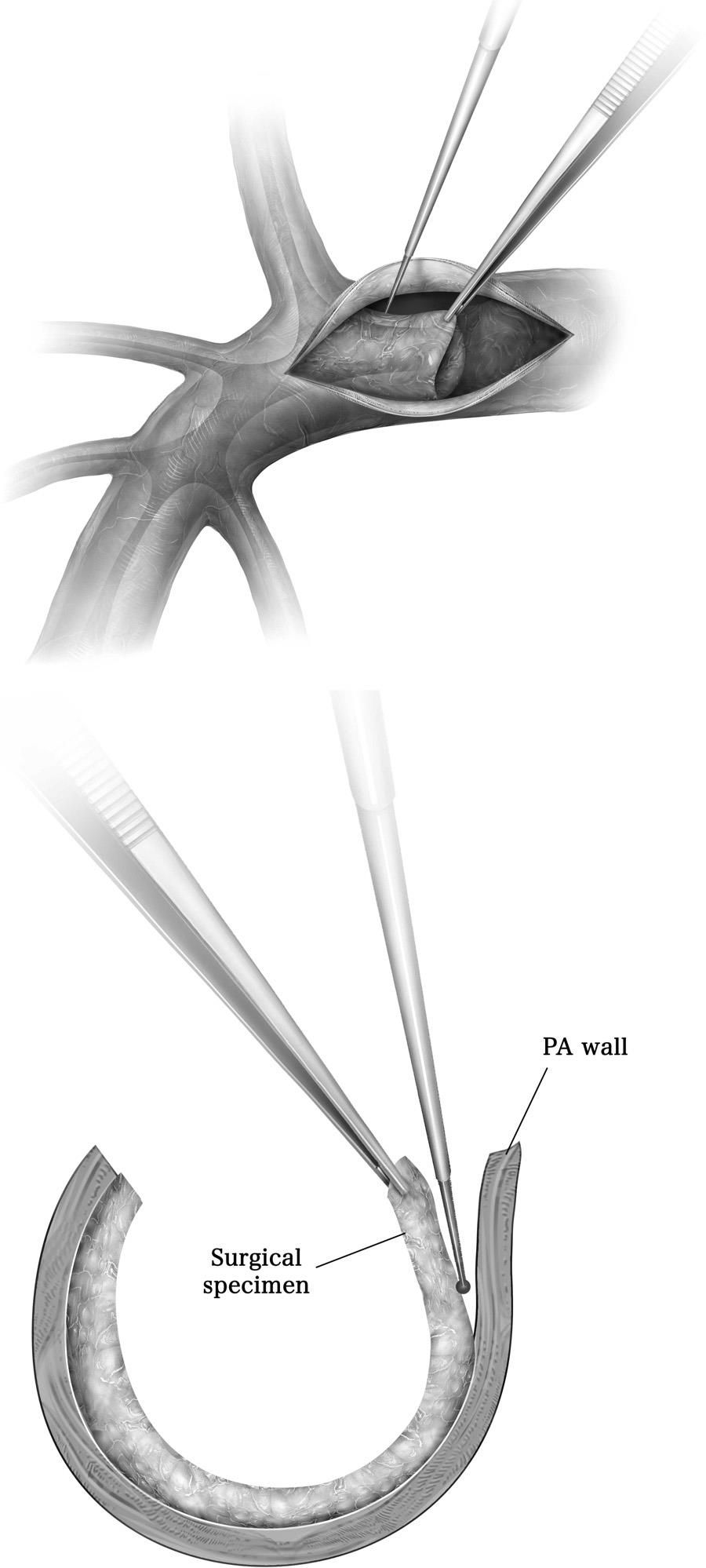
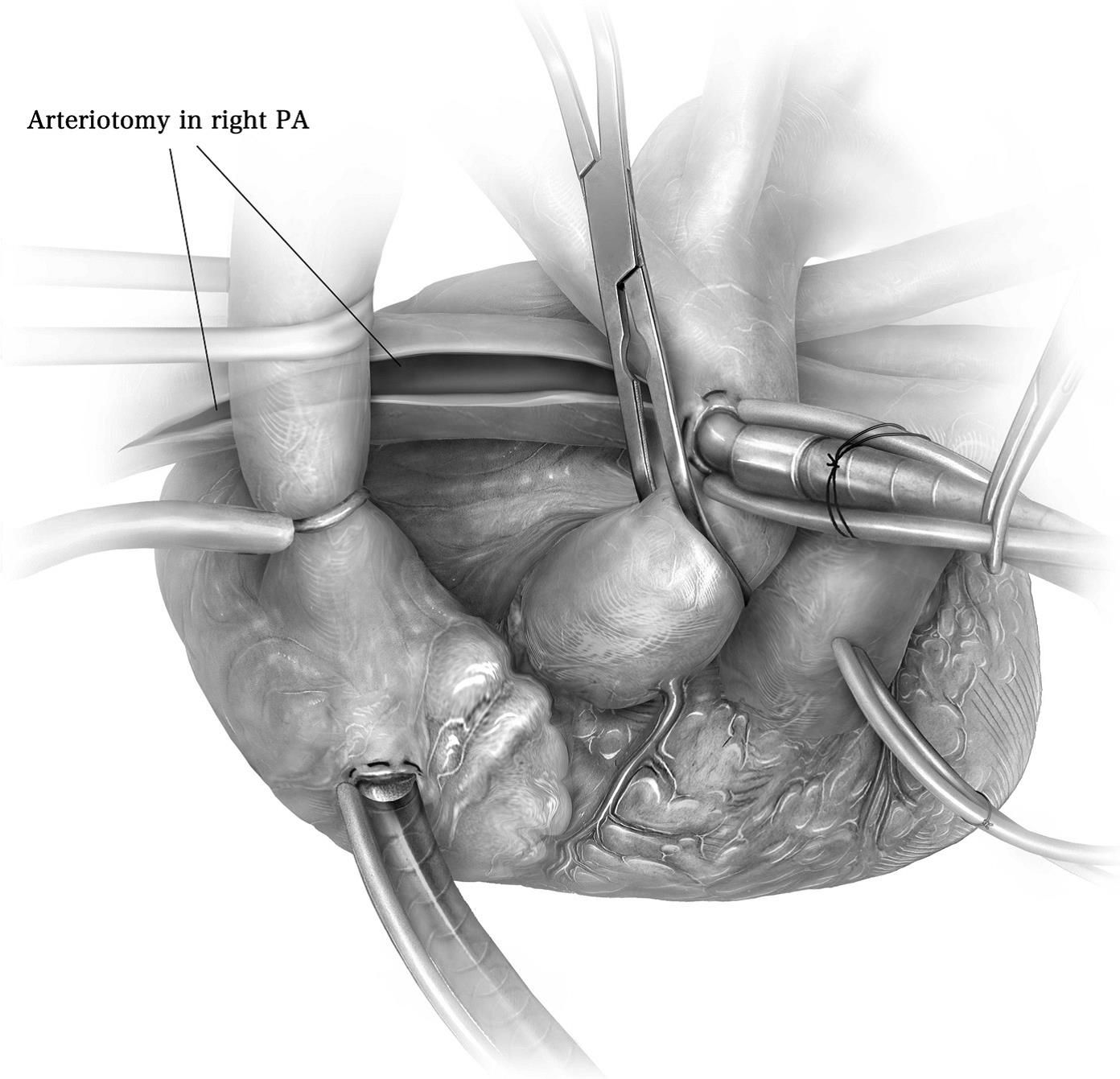
During the operation, the vessel wall is opened with a small incision in the middle of the main trunk of the pulmonary artery in the area of the sternum after opening the chest (Fig. 3). The three-part arterial wall on the right side is then cut open in its entire circumference between the inner and middle layer (Fig. 4). The surgeon then works his or her way along the vessel wall in this layer as far as possible to the second or third division of the right pulmonary artery. This is extremely delicate, as the view is naturally very restricted and the surgeon must rely on his or her excellent anatomical knowledge and experience. If the layer is lost too early, the pulmonary artery can only be opened inadequately or, in the worst case, the vessel wall can even rupture.
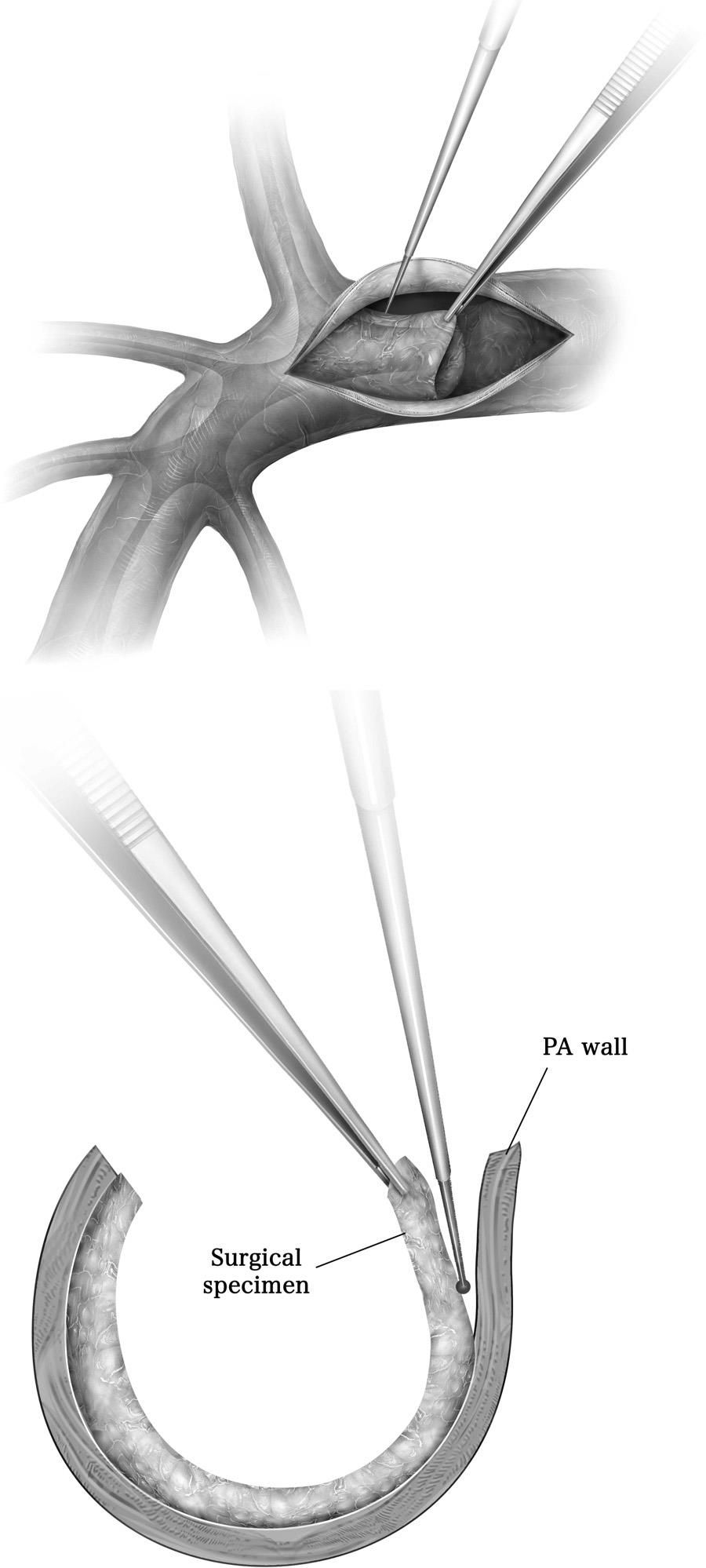
Stripping the material
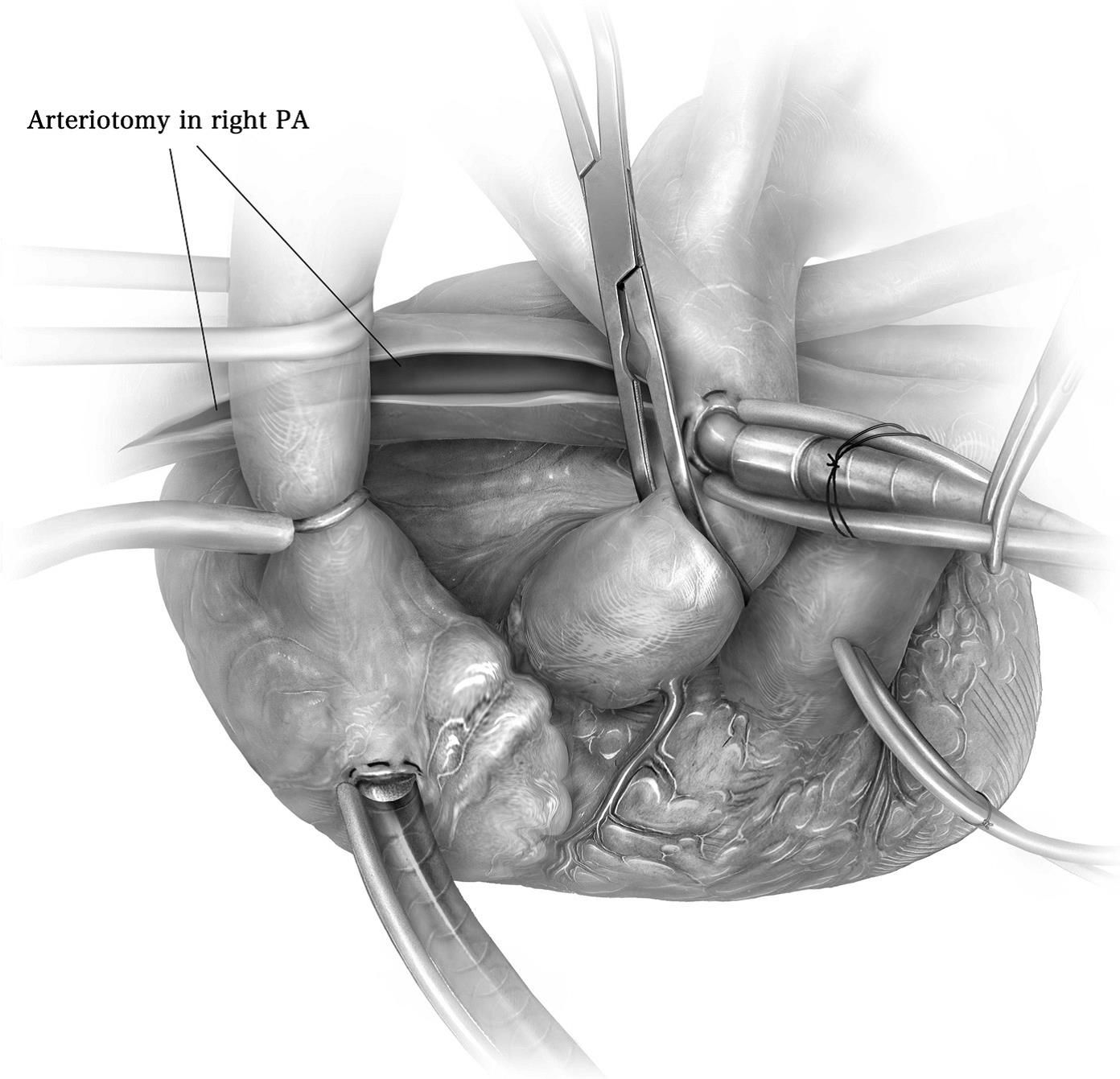
Endarterectomy of the right pulmonary artery
In most cases, however, surgery succeeds in working its way up the vessel wall to the third division of the pulmonary artery or even further and then removing what could be described as an outflow of the entire arterial tree, including the inner part of the arterial wall (Fig. 5). It is important to point out that the surgeon does not simply remove the clot from the pulmonary artery, but also the inner part of the arterial wall.

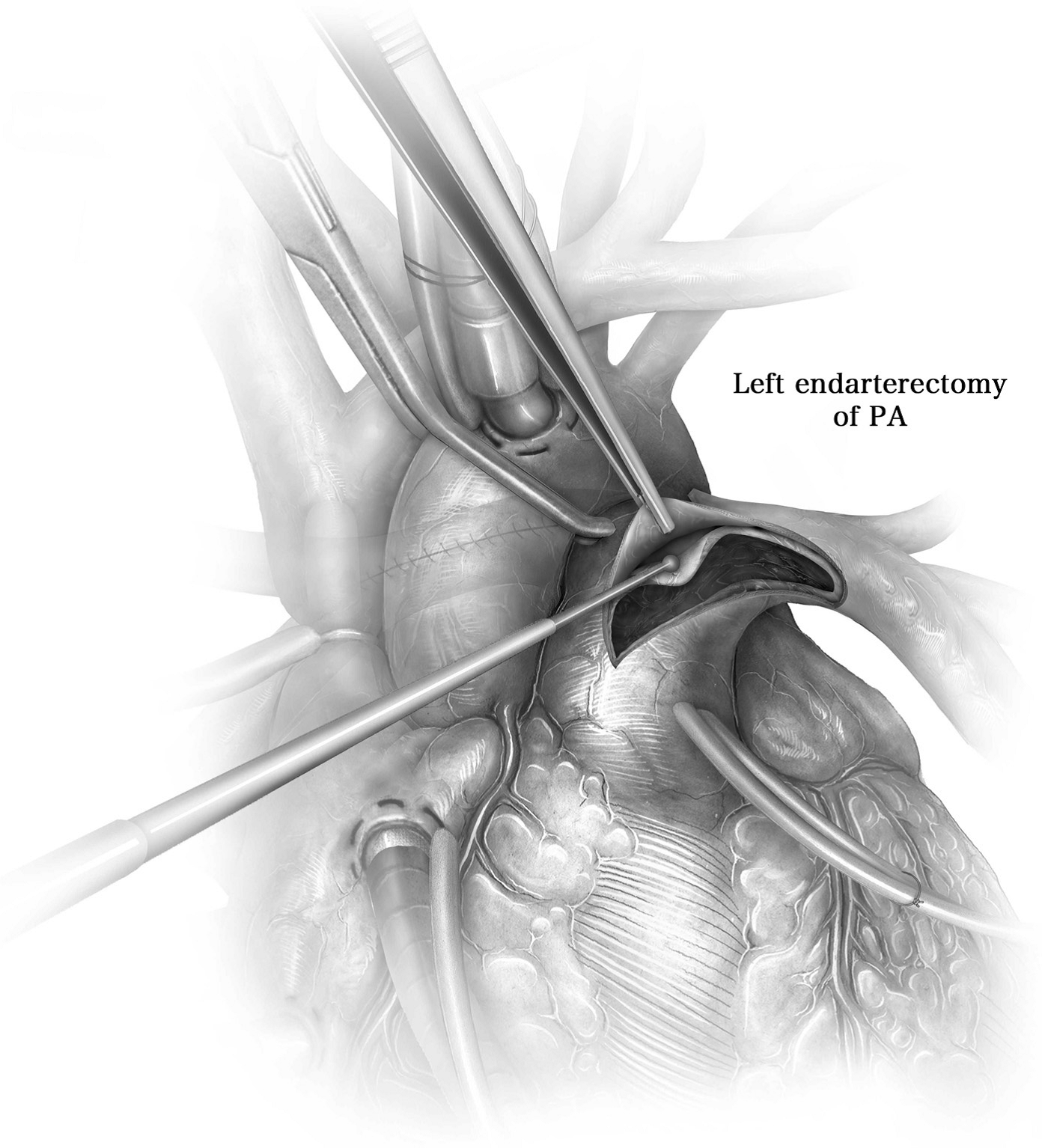
Removed arterial tree including the arterial wall
Since, as mentioned above, the lungs are also supplied with blood by the systemic circulation and the blood flowing back into the pulmonary artery from this systemic circulation would massively impair the surgeon’s vision, the operation must be performed in total circulatory arrest. This is done on the heart-lung machine, where the patient’s body is cooled to a temperature of 18°C. The head is also cooled from the outside. Then, shortly before the incision in the pulmonary artery, the heart is stopped and finally the heart-lung machine is also switched off, i.e. a total circulatory arrest is produced. The actual operation described above takes an average of 20 to 30 minutes. Circulation is then restored for a short time and the left pulmonary artery is operated on in the same way (Fig. 6). Afterwards, circulation is restored and the patient’s body is slowly warmed up. While the actual endarterectomy takes two times twenty minutes, the entire operation, including preparation of the artificial circulation, cooling, circulatory arrest and rewarming of the patient, takes around eight hours.
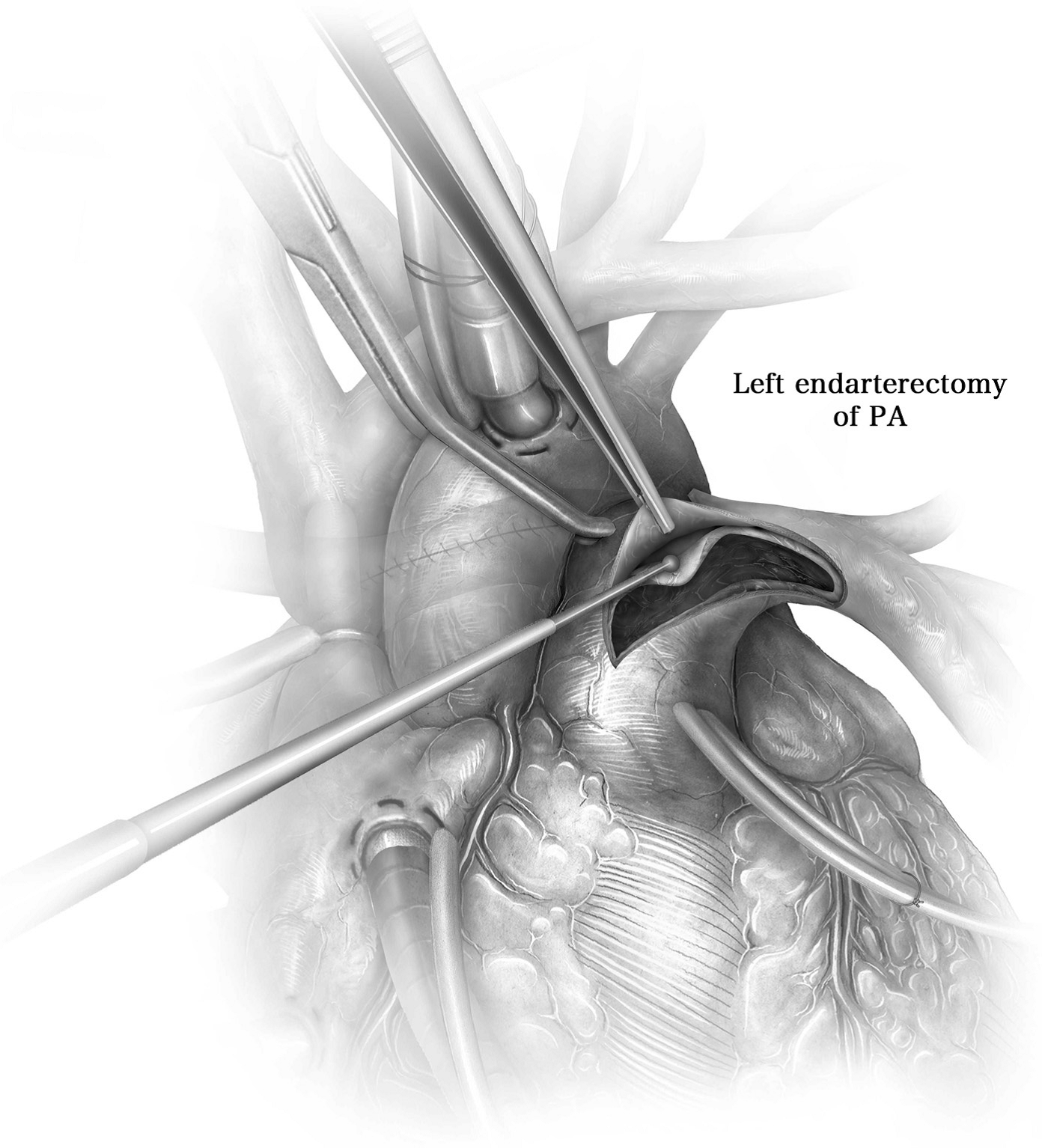
Endarterectomy of the left pulmonary artery
PEA is a difficult and complex operation. Up to 10% of patients die during the operation. However, the most experienced surgeons in the world today achieve a mortality rate of less than 5%. The main causes of death are acute bleeding, for example when the pulmonary artery ruptures during dissection of the vessel wall, and so-called reperfusion edema. This is an accumulation of fluid in the lungs after surgery as a result of increased blood flow to areas of the lungs not previously supplied by the circulatory system. While the first complication is difficult to control, reperfusion edema can often be controlled after several days of ventilation. Other immediate postoperative problems include acute kidney failure and confusion in around 5 to 10% of patients. If the operation proceeds without complications, the patient can usually be weaned off artificial respiration after one or two days and leave the hospital after two to three weeks. In most cases, a two- to three-week rehabilitation stay is then planned.
PEA enables most patients to return to practically normal performance. Of course, as a result of the often very long course of the disease up to PEA, there is a severe lack of fitness. In around 10 to 20% of cases, the pulmonary pressure cannot be completely normalized by PEA, which is why the patient’s performance remains limited – but not to the same extent as before the operation. Some patients still require drug therapy after the operation.
The procedure is such that we carry out the preliminary investigations (cardiac ultrasound, gait test, pulmonary function test, pulmonary angiography, CT perfusion scintigram, right and left heart catheterization) in collaboration with the pulmonary hypertension consultation and discuss the documents on an interdisciplinary basis. In particular, pulmonary angiography and computed tomography are analyzed with regard to the distribution and surgical accessibility of changes in CTEPH. The following can be assessed: 1) whether an operation is possible at all, 2) how well the changes can be achieved by the surgeon, i.e. how difficult the PEA, and therefore the perioperative risk, will be and 3) what is the approximate chance that most of the changes can be removed and what is the approximate prognosis regarding the improvement in performance after the operation.
We will then organize another consultation in the CTEPH clinic, where we will explain the situation to you in detail. It’s worth seeking advice even if you don’t want an operation! Neither the clarifications nor such a discussion anticipate anything; you can then make your own independent decision. We therefore advise all patients to have tests carried out, regardless of their personal attitude. It is also possible to talk to someone who has already had a PEA.
“Puls” accompanied a patient, Prof. Schmitt-Optiz and her team during this extraordinary procedure. SRF Puls – Extreme surgery