Overview: What is acne inversa?
Despite the similar name, acne inversa (acne inversa) should not be confused with “common acne” (acne vulgaris), which plagues many adolescents during puberty. Rather, it is a chronic skin disease that is difficult to treat and in which painful and often weeping skin changes (skin lesions) form on various parts of the body, usually in episodes.
Rupture, Alexander Navarini
Acne inversa – frequency and age
In Western Europe, an estimated one percent of the population suffers from acne inversa. Women are more frequently affected than men. The disease usually breaks out in early adulthood, more precisely after puberty and before the age of 30. In principle, however, acne inversa can occur at any age.
Acne inversa: causes and risk factors
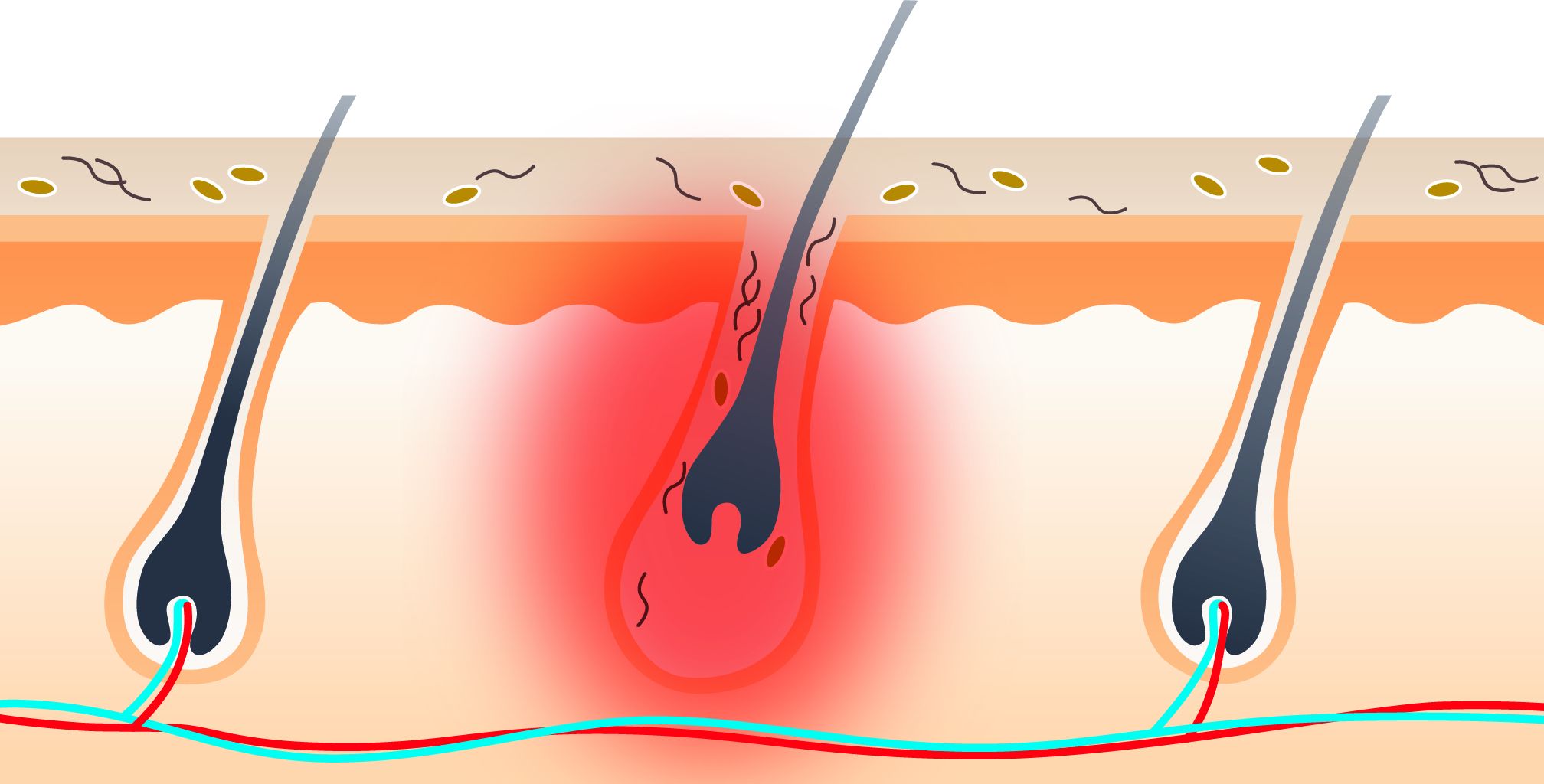
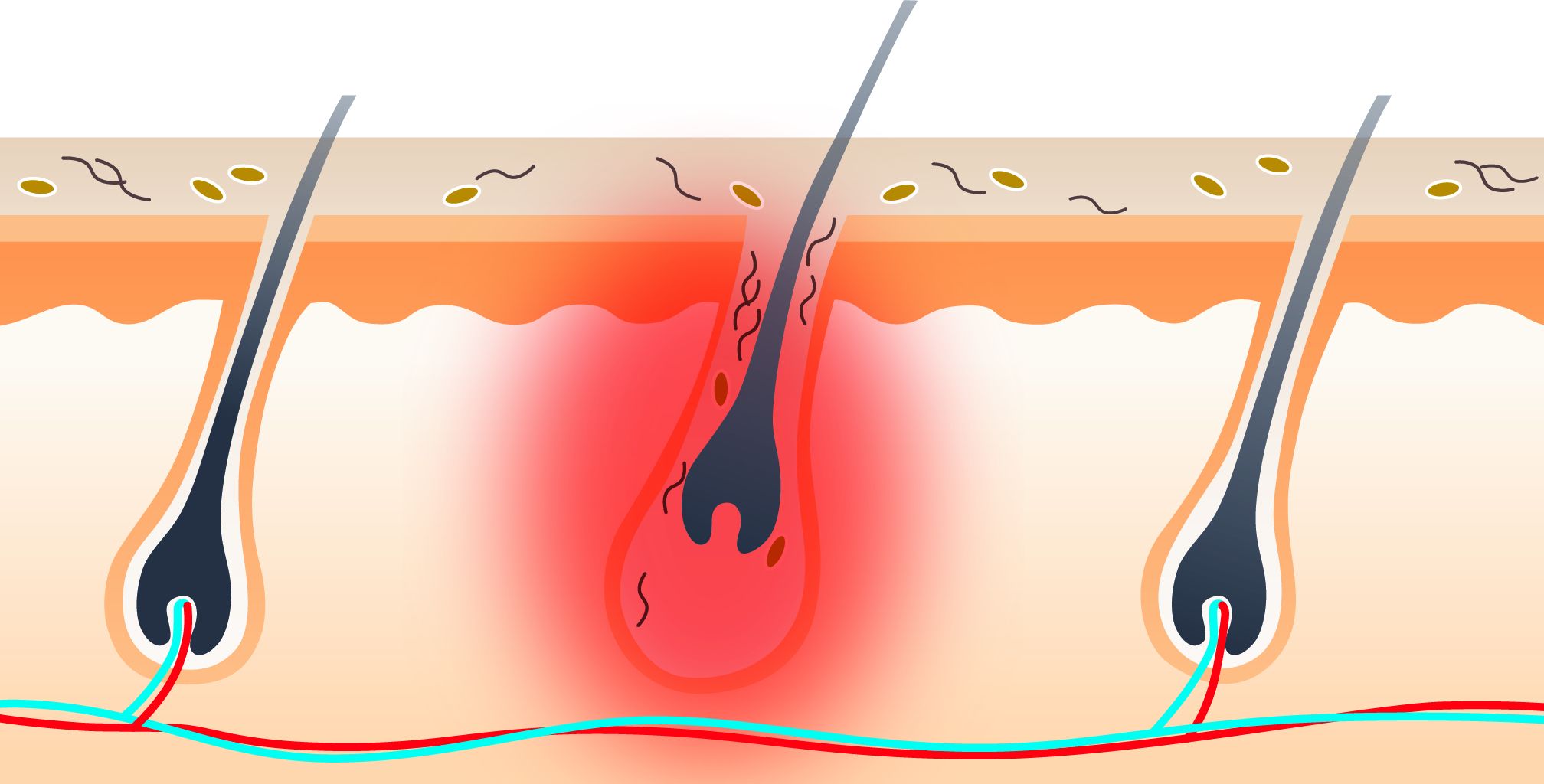
A central role in the development of acne inversa appears to be played by a thickening of the horny layer (hyperkeratosis) in the area of the hair follicles. As a result, the confluence points of neighboring sebaceous and sweat glands can become blocked. Sebaceous and sweat secretions accumulate, causing deep-seated local inflammation – including the formation of painful nodules and encapsulated accumulations of pus (abscesses).
The exact causes of these severe skin changes are not yet known. However, several factors are probably involved in the development of acne inversa. We assume that there is a genetic predisposition to the disease because it sometimes runs in families. In combination with other factors, it could then erupt. The following triggers for acne inversa have been proven or are under discussion:
- Smoking
- Severe overweight (obesity = adiposity)
- Excessive sweating(hyperhidrosis)
- Mechanical irritation of the skin (e.g. from shaving)
Acne inversa – often associated with other diseases
Acne inversa occurs more frequently in the context of certain other diseases. These include, for example, the two chronic inflammatory bowel diseases Crohn’s disease and ulcerative colitis as well as rheumatic diseases.
Symptoms: Acne inversa
Typically, acne inversa causes painful, bright red, firm skin nodules and skin lumps. These can develop into encapsulated collections of pus (abscesses), which can fuse together in the depths and burst outwards. Then purulent or bloody-watery secretions come out. The skin changes can disappear spontaneously, but can recur and also persist. In addition, branched tubular ducts can form in the tissue, so-called fistulas. They can open out on the surface of the skin and secrete a secretion. When the inflammatory skin changes heal, they often leave scars.
Acne inversa: three degrees of severity
Depending on the severity of the disease, we differentiate between three stages (Hurley Score):
- Stage one: single abscesses, no formation of fistulas and scarring
- Stage two: one or more widely separated abscesses, plus fistula tracts and scarring
- Stage three: extensive infestation with abscesses, fistula tracts and scarring
Acne inversa: Which areas of skin are affected?
The inflammatory skin changes in acne inversa mainly affect areas of the body that have skin folds or where areas of skin rub against each other. These mainly include:
- Armpits
- Groin area
- Genital and anal region
Sometimes the inflamed areas of skin can also be found on other parts of the body, such as under the breast (in women) or on the inside of the thighs. The face, hairy scalp and back are only rarely affected.
Online skin check: Quick and convenient from home
Send a photo of the affected skin area and fill out the short questionnaire. Within 24 hours on weekdays, you will receive a reliable diagnosis from our experts. Your data will be transmitted to us encrypted and treated confidentially.
Diagnosis of acne inversa
First, we will talk to you in detail to get a picture of your medical history (anamnesis). Possible questions include:
- What are your symptoms?
- When did you notice the first skin changes?
How have they changed since then?
- Are there any known cases of acne inversa in your family?
- How tall are you and how much do you weigh?
- Do you smoke?
We can calculate your body mass index (BMI) from your height and weight. This then indicates whether you are overweight. As mentioned above, being overweight – just like smoking – has a favorable effect on acne inversa.
The medical history interview can be followed by various examinations, although not all of them are necessary in every case:
- Examination of the affected skin areas.
We carefully examine the inflamed areas of skin.
If necessary, we will examine fistula tracts more closely by inserting a small probe into their mouths.
- Swab.
In order to prove the involvement of bacteria in the inflammatory processes, we can take a smear from deeper tissue areas and send it to the laboratory for analysis.
- Blood test.
Sometimes we take a blood sample to determine inflammation values such as the C-reactive protein (CRP).
- Imaging procedures.
In some cases, ultrasound or magnetic resonance imaging (MRI) is used to examine how deep the inflammation has spread into the tissue.
These examinations can not only help to confirm the suspicion of acne inversa, but also to rule out diseases with similar symptoms. These so-called differential diagnoses in acne inversa include, among others:
- Recurrent inflammation of hair follicles (folliculitis)
- Boils (painful purulent inflammation of a hair follicle and the neighboring tissue)
- Carbuncle (deep, painful, joint inflammation of several adjacent hair follicles)
- Skin tuberculosis
- Trichophytosis (infection of the skin and its appendages – such as hair – by fungi of the genus Trichophyton)
- in the anal area, e.g. anal fistula and Crohn’s disease
In summary, the path to a correct diagnosis of acne inversa is often long. It is not uncommon for the disease to be diagnosed and treated years after its onset. One reason for this is that many sufferers delay contacting a doctor out of shame. In addition, the diagnosis of acne inversa is often difficult. The skin changes of this serious disease are sometimes mistaken for ordinary abscesses or attributed to an inflammation of the hair follicle (folliculitis), especially in the early stages.
Acne inversa: prevention, early detection, prognosis
As the exact causes of acne inversa are not yet known, the disease can hardly be effectively prevented. However, if you have a family history of acne inversa, it may be beneficial to avoid known risk factors such as smoking or being overweight.
Acne – progression and prognosis
Acne inversa is a chronic disease that usually progresses in phases. Treatment can improve the symptoms, but not cure them. Even after surgical removal of affected skin lesions, abscesses and other skin changes can occur again later.
Complications are rare with acne inversa. These include, for example, erysipelas and swelling due to accumulated lymph fluid (lymphoedema). It is also rare for the skin lesions of acne inversa to develop into a certain form of skin cancer (squamous cell carcinoma).
As severe as the physical symptoms of acne inversa can be, the associated psychological stress should not be underestimated. It can lead to those affected withdrawing from social life and even becoming depressed.
Acne inversa: treatment is planned individually
The treatment for acne inversa depends largely on the severity of the disease.
It can include various medications and/or surgical interventions.
Details of the treatments