Overview: What is bronchial asthma?
Bronchial asthma is a chronic inflammatory disease of the airways. This means that the airways react very sensitively to different stimuli by contracting and constricting. In addition, the mucous membranes in the bronchial tubes swell and can develop thick mucus. The respiratory muscles cramp, resulting in acute respiratory distress.
Bronchial asthma should not be confused with “cardiac asthma”, in which fluid accumulates in the lungs due to weakness of the left ventricle.
Frequency: Bronchial asthma is widespread in Switzerland
The incidence of bronchial asthma varies from country to country. It is highest in Sweden, England and the Netherlands, with a frequency of between 15 percent and 20 percent. Bronchial asthma is also widespread in Switzerland: Every tenth child and every 14th adult suffers from it. Allergic asthma is more common in children, whereas non-allergic causes are more likely in adults.
Causes and risk factors: Natural and artificial allergens
The causes of bronchial asthma are divided into two large groups: Allergic asthma and non-allergic asthma.
Allergic bronchial asthma
Allergic bronchial asthma, also known as extrinsic asthma, is an allergic reaction to certain substances in the environment (allergens) that are not normally harmful. These allergens include, for example
- Pollen,
- Animal hair and bird feathers and
- House dust mites or mold spores.
Certain foods can also trigger allergic bronchial asthma; however, this is usually accompanied by other symptoms such as itching in the mouth, runny nose, conjunctival irritation and/or urticaria, for example:
- Seafood
- Nuts
- Peanuts, soy and other legumes
- Glutamate in ready meals
- Stabilizers such as sulphites in wine, fruit juices, dried fruit and canned fish
Finally, medication can also trigger asthma symptoms – painkillers such as acetylsalicylic acid and other rheumatic painkillers are primarily responsible for this.
It is also known that the hypersensitivity of the airways in allergic asthma is hereditary. If one parent suffers from allergies, 30 to 40 percent of children are also affected. If both parents are allergic, their children have a 60 to 80 percent risk of also developing allergies.
Non-allergic asthma
Non-allergic asthma, also known as intrinsic asthma, is caused by other stimuli and usually begins after the age of 40. Typically, the paranasal sinuses are chronically inflamed in this form of asthma. Severe forms are often found.
Symptoms: whistling, life-threatening shortness of breath
Typically, bronchial asthma manifests itself with asthma attacks following contact with an allergen or irritant. If there are only a few minutes between contact and seizure, experts speak of an immediate-type reaction. If several hours pass before the affected person has asthmatic symptoms, this is considered a late reaction.
The hypersensitive reaction of the airways is caused by a combination of thick mucus, narrowing of the airways and cramping of the respiratory muscles. This causes seizures with the following possible characteristics:
- Sudden, severe shortness of breath with a whistling sound when exhaling
- Tightness in the chest and fear of suffocation
- Acceleration of breathing and heart rate
- Persistent cough with thick sputum
- Bluish lips and face due to lack of oxygen and cold sweat
An asthma attack can last seconds or several hours. If the asthma attack lasts for days, experts speak of a “status asthmaticus”.
Diagnosis of bronchial asthma
Skin tests, inhalation provocation tests and lung function tests
In order to make a diagnosis of bronchial asthma, we first need a detailed medical history. Most people affected complain of acute attacks of breathlessness. We will ask you when, where and how exactly the seizures occurred. We also try to establish a connection with a possible allergen. The diseases in your family are also interesting. We will want to know if there are any family members with a diagnosis of bronchial asthma.
We will listen to your lungs and initiate further examinations, for example:
- X-ray examination of the lungs
- Special blood tests: These can be used, for example, to detect elevated antibody levels to allergens in the blood.
- Skin tests: They help to find the triggering allergen.
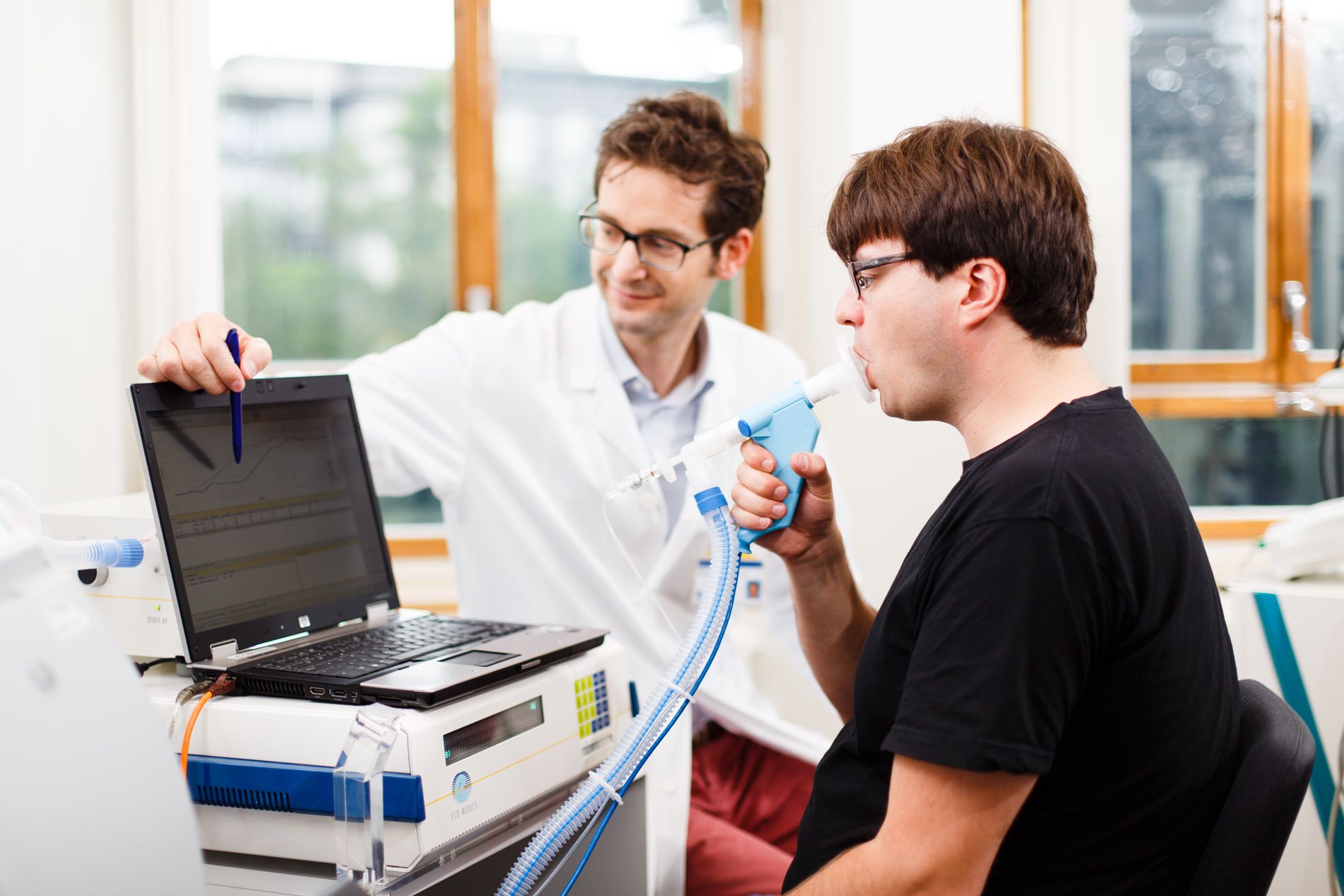
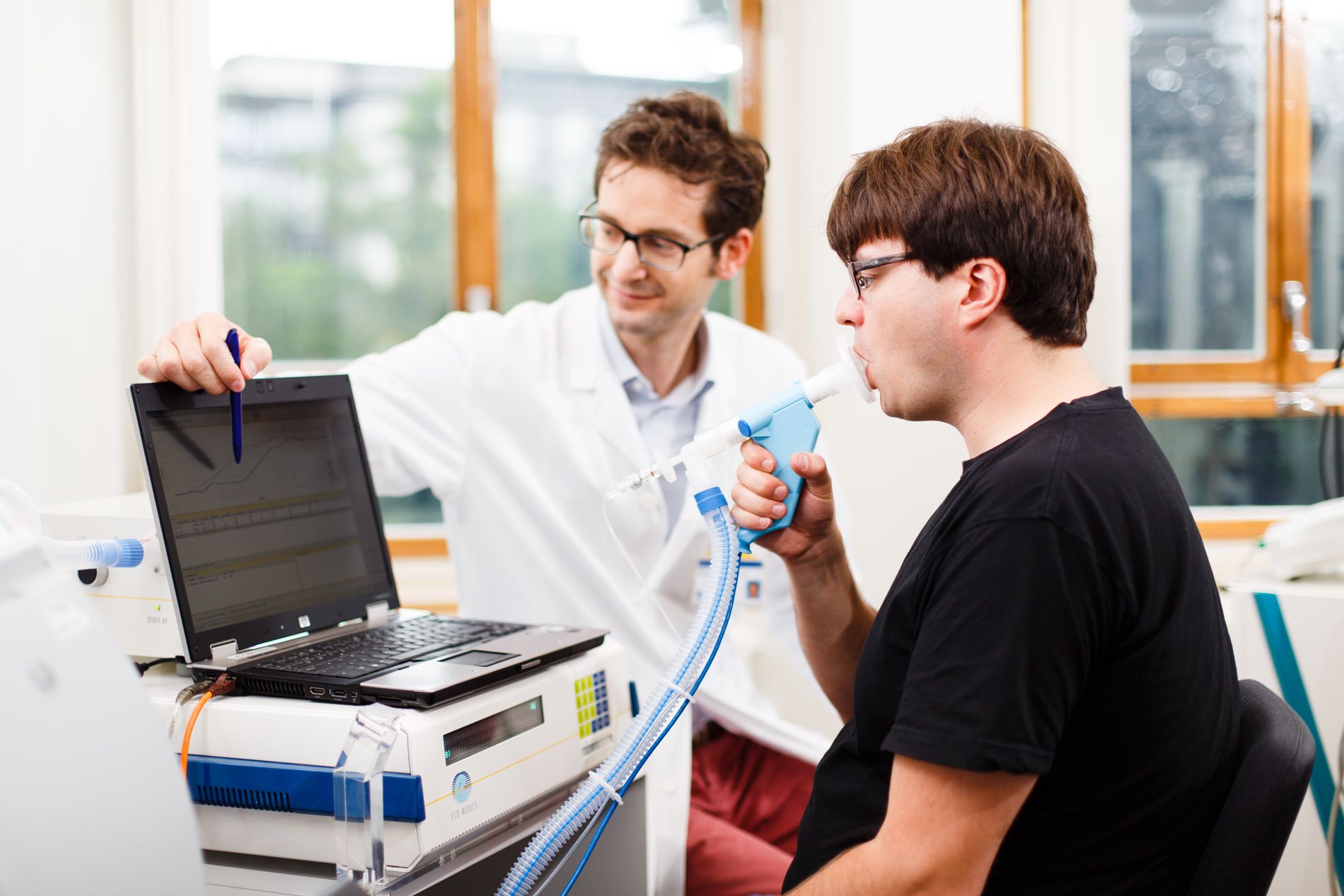
- Lung function test such as spirometry: Spirometry is the measurement and recording of respiratory volume and airflow velocities to assess lung function. You simply breathe in and out via a mouthpiece-tube system.
- FENO test: This is a determination of nitrogen monoxide in exhaled air. This provides valuable information about the inflammatory state of the lungs. FENO is the abbreviation for fractionated exhalednitric oxide(NO).
- Computed tomography (CT ) of the lungs: CT allows the airways and changes in the lung parenchyma to be visualized. As the examination is carried out both inhaling and exhaling, regional differences in ventilation can be detected at an early stage.
- Magnetic resonance imaging (M RI) of the lungs: MRI allows the measurement of regional oxygen exchange (OE-MR, oxygen-enhanced MR) and thus provides direct indications of how severely certain areas of the lungs are affected.
Prevention, early detection, prognosis: avoid triggers!
If you suffer from bronchial asthma, you can protect yourself from new asthma attacks by avoiding the triggers. Depending on what triggers the disease, the following measures are helpful:
- Do not smoke and keep your distance from smokers.
- Avoid spending time outdoors during the pollen season.
- Inflammation of the airways must be diagnosed and treated by us in good time.
- If you are allergic to animal hair, it is advisable not to keep pets.
- Consistently avoid foods that cause allergic asthma.
- Use allergen-free mattresses and comforters.
- Ensure the right humidity in a room because dry air irritates the airways.
- Drink plenty of water to help clear the mucus in the bronchial tubes.
- Avoid antibiotics and painkillers that trigger allergies.
- In the case of respiratory allergies, so-called hyposensitization (immunotherapy) can be useful under certain circumstances.
In the event of an asthma attack, you should carry emergency medicine and emergency documents with you. We will equip you accordingly.
Progression and prognosis: good with the right treatment
Timely and personalized treatment is important for the course and prognosis of the disease. Children with allergic asthma who are treated correctly have a chance of being free of symptoms in childhood and adulthood. Without therapy, asthmatic crises damage the airways in the long term and impair the lungs’ ability to function. If bronchial asthma is not treated correctly, the constant strain on the lungs and heart can lead to complications such as pulmonary emphysema, an irreversible over-inflation of the alveoli.